Telehealth promised to make healthcare more convenient and accessible, but delivering on that promise has proven difficult. Awkward interactions, uneven care quality, and wait times add new layers of complexity to virtual care instead of stripping them away.
The integration of AI in telemedicine finally gets telemedicine closer to what it promised: seamless, patient-centered care, whenever the patient can access it.
How is telemedicine feeling these days?
Telemedicine services seem to be growing robustly, fuelled by increasing patient demand, rapid tech advancements, and loosened regulations:
- Between 2024 and 2028, the virtual doctor consultations segment of the digital health market was projected to grow by 11.7% to 13.7 million users.
- In 2024, the global telehealth market size was $123.26 billion and is projected to grow at a CAGR of 24.68% from 2025 to 2030.
- According to the American Medical Association, 74% of physicians work in practices that offer telehealth.
But looking closer at the user sentiment toward virtual care, we’ll see a more nuanced and conflicting image:
- A study of over 2,100 physicians found that healthcare professionals who conducted more telemedicine visits also experienced additional work related to Electronic Health Records (EHRs) outside of regular appointment times.
- Almost 80% of primary care physicians and 56.3% of specialists reported an increase in their workload due to telehealth messaging.
- Around 25% of patients are dissatisfied with the limited services provided via telemedicine.
Also, telehealth startups are fighting for survival — not just with each other, but with retail clinics too. So for telehealth innovators, it’s time to reinvigorate their offerings and drive engagement through new sources of consumer value.
How AI enhances telemedicine: 7 high-value use cases
By 2033, the global AI in telemedicine market size is expected to surpass $193 billion, compared with $18.39 billion in 2024. This 950% growth is not surprising. Without AI, virtual care would remain a watered-down version of in-person visits, full of guesswork, inconsistent care, and admin overload.
Virtual health assistants
Human expertise remains central even as AI tools augment care. However, today’s patients demand instant answers at midnight, on weekends, and during lunch breaks. Powered by conversational AI, AI virtual assistants can fill communication gaps when clinicians aren’t available:
- Medical guidance — Virtual healthcare assistants and agents, such as those provided by K Health and Amwell, offer expert-backed, on-demand answers to health questions, using patient EHR data to inform recommendations.
- Triage and follow-up — Conversational interfaces, such as Dokbot by Doxy.me, help physicians collect data from patients before conducting a virtual visit and automate post-appointment check-ins based on wearable device trends.

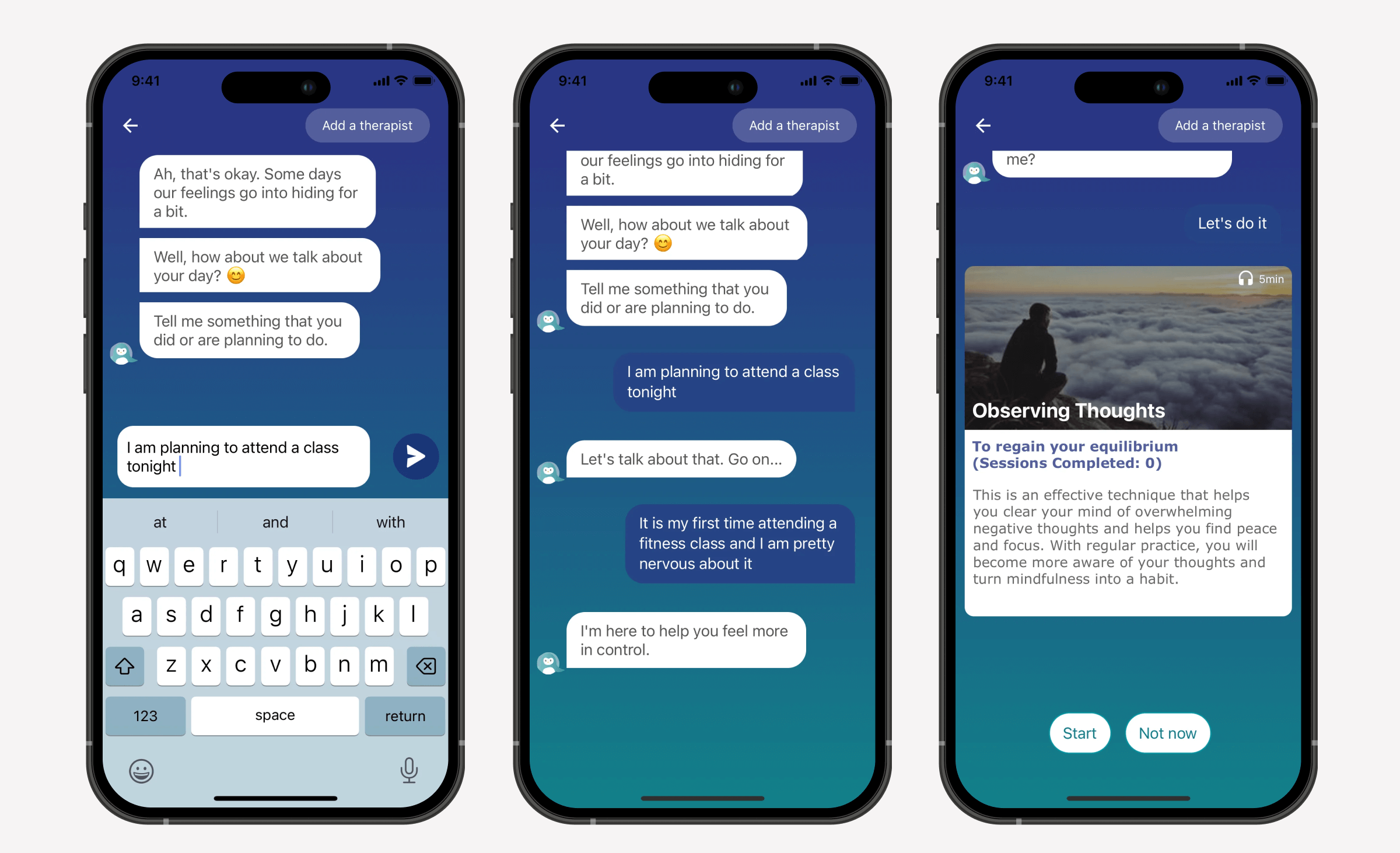
- Mental health support, chronic condition care, and patient self-management — Whenever users feel the need for a supportive, expert-backed companion, virtual assistants such as those in Talkspace Go and Meru Health can offer on-demand therapy access, combining behavioral or chronic condition support with human escalation.
Faster, smarter diagnoses
Remote healthcare delivery, although convenient, comes with a significant downside: the lack of physical interaction often eats into diagnostic accuracy. On the other hand, IoT-enabled virtual care allows for continuous monitoring of patients’ health, but without artificial intelligence analytics, this longitudinal data will remain untapped.
Depending on the exact combination of technologies (natural language processing, predictive algorithms, etc.) and data sources (electronic health records, patient-reported input, etc.), artificial intelligence can power different types of features for diagnostic support:
- AI-assisted symptom interpretation — By leveraging NLP capabilities, telemedicine apps, such as Ada Health and HealthTap, can perform symptom triage, risk stratification, and pattern-based condition screening to determine a patient’s health state.
- Visual data analysis — Healthy.io, TytoCare, and SkinVision enable at-home diagnostic testing, dermatologic triage, and contactless vital monitoring — all the courtesy of computer vision.
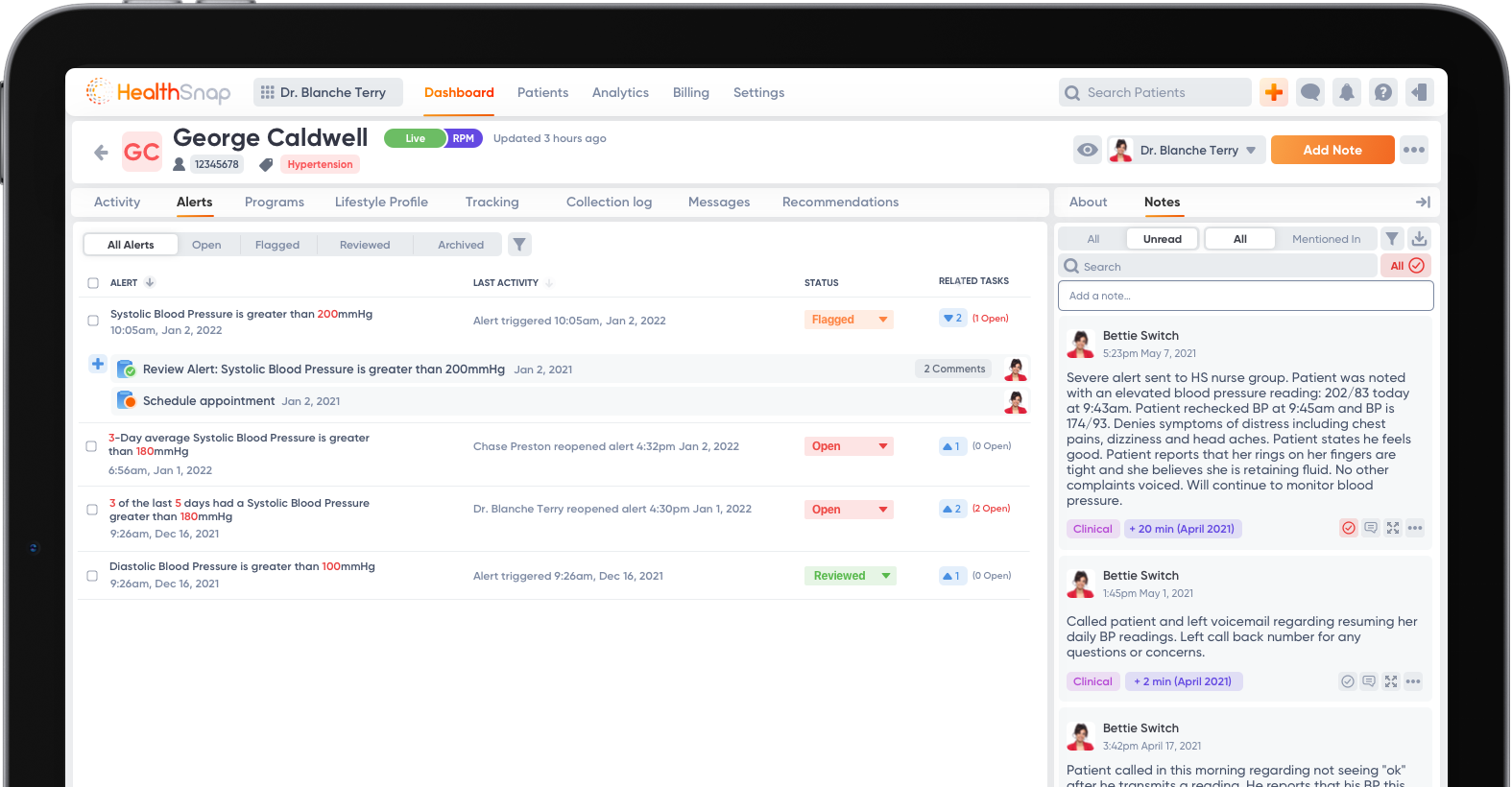
- Analysis of vital signs — By funneling extensive patient data from wearables and remote patient monitoring devices, apps such as HealthSnap, CareSimple, and Vivify Health help clinicians monitor patients between virtual visits and obtain a comprehensive view of a patient’s health before a visit.
- Augmented clinical decision support — Making sense of EHR medical data, visit notes, and RPM vitals, apps like Teladoc, MDLive, and 98point6 function as diagnostic assistance and predict patient outcomes.
Intelligent admin
As we mentioned earlier, without AI tools, telemedicine apps create an additional administrative burden, not just for clinicians but for the entire care ecosystem. By integrating AI into telemedicine, healthcare providers can reclaim their time and automate administrative tasks that are time-consuming and detract from patient care.
Artificial intelligence and machine learning algorithms do that in multiple ways:
- Smart intake and scheduling — AI algorithms inside platforms such as Mend, eVisit, and Allara handle appointment booking, reschedule appointments, verify insurance, and connect a patient with the right provider based on the symptoms, location, and availability.
- Automated clinical documentation — For healthcare professionals, AI scribes such as Abridge, Suki AI, and hellocare.ai reduce notetaking time, allowing clinicians to perform at the top of their license.

- EHR data extraction and summarization — Same AI scribes can extract critical medical data from EHRs before a visit, so clinicians don’t have to frantically read through a load of patient information during a 15-minute call.
- Automated coding and compliance — Integration with ambient AI tools, such as Nuance Dragon Ambient eXperience, can also extend the capabilities of telemedicine apps to feature AI-based documentation checks, medical coding, and compliance risk detection.
Language and accessibility support
According to a study, older adults in the US with vision impairment have difficulty accessing digital technology, including telemedicine. Individuals with disabilities, people with limited English proficiency, and those with limited digital literacy may also be at a disadvantage when it comes to alternative care options.
Telemedicine apps can leverage the AI-powered capabilities of third-party tools to make virtual care services inherently accessible for everyone:
- Real-time translation and visual captioning — LanguageLine, Google Live Translate, and other AI-driven translation engines supplement telehealth apps with dynamic, context-aware translation of both text and speech.
- Dynamic language simplification — GPT-based virtual assistants and chatbots can rewrite clinical narratives in simpler language in real-time.
- Visual interpreting for blind/low-vision patients — Although it’s an emerging use case, tools like Be My Eyes, paired with conversational interfaces, help patients with visual impairments describe their visual symptoms to doctors and understand clinical documents.
Mental health screening and support
Telemedicine has made at-scale behavioral healthcare services more accessible, but artificial intelligence has taken it to the next level. AI-based tools fill in when therapists are unavailable, create a safe, stigma-free space for individuals, and act as an extra layer of clinical decision support for mental health professionals.
In telemental health applications, artificial intelligence enhances care and patient outcomes through:
- AI-based mood and behavioral analysis — With sentiment analysis and natural language processing at the heart, Wysa, Quartet Health, and other remote care applications detect signs of depression, anxiety, and other mental health symptoms based on users’ word choice, tone, and conversational patterns — and route users to human therapists, if needed.
- Stigma-free screening via passive monitoring — Users who feel uncomfortable sharing their thoughts and emotions with a therapist might benefit from AI tools that collect data, like sleep patterns, facial expressions during check-ins, and voice biomarkers, in the background to analyze the state of mental health.
- Crisis support — In apps like Talkspace, AI-enabled interfaces function as a 24/7 crisis triage layer, searching text messages for urgency and linguistic red flags. Based on specific triggers, the system notifies therapists and suggests crisis resources to individuals in real-time.
End-to-end care orchestration
Instead of focusing on a narrow care space, telemedicine applications can go beyond episodic virtual visits to meet patients’ care needs across specialties and phases. However, a more comprehensive care continuum requires a layer of smart coordination to integrate the patient’s fragmented care context into a unified clinical narrative.
Unmatched analytics capabilities of AI tools lend themselves well to this task. In telemedicine apps, AI-enabled collaborative care delivery is supported by:
- Dynamic, longitudinal care plans — Platforms such as Allara and Jasper Health integrate disparate data from multiple care touchpoints, including video visits, wearable data, lab results, and more, into a harmonized interface to create a single care plan for managing chronic diseases, mental health conditions, and other conditions.
- Continuous feedback loops — To ensure care plans evolve in real time as patient data changes, remote care solutions such as Bioformus, Vivify Health, and BetterHelp, among others, rely on artificial intelligence to provide real-time updates from wearables, RPM devices, and patient-reported outcomes, thereby adjusting care plans and therapy session frequency in real time.

- Whole-person care support — Using AI-driven patient data analysis, holistic remote care platforms like Maven Clinic piece together a comprehensive picture of patients’ mental, physical, and social care needs to ensure high-impact care experiences.
Tailored care journeys and behavioral nudging
Just like fitness app users need motivation to stick with workouts and healthy meals, telemedicine users can rely on gentle, personalized nudges and other engagement features to stay committed to their treatment plans and medication regimens.
Although personalization is not entirely reliant on AI, machine intelligence enhances the speed, scale, and depth of personalized care experiences, enabling telemedicine apps to make all users feel heard and seen. Examples include:
- Tailored medication reminders — Telemedicine applications that include a dedicated AI medication management module help users stay on their prescribed medications with contextual reminders sent at the right time and frequency. For example, DrChrono’s telemedicine module integrates with Medisafe, a medication management app, to enable this functionality.
- Chronic condition self-management — Tailored health prompts can also become a key component of long-term condition management, providing users with the insights, guidance, and motivation to care for their health consistently. Usually, this type of intelligence is based on data streams from connected medical devices — the same approach as used in Livongo’s Health Nudges.

- Mental health management and relapse prevention — By breaking down user engagement patterns and emotional cues during therapy sessions, apps like SilverCloud by Amwell and Headspace fine-tune the content and exercises to match a patient’s current state.
- Pre- and post-operative care pathways — Surgical care telemedicine platforms also employ personalization to tailor care plans to the patient’s unique needs during pre-operative preparation and post-operative rehabilitation. Kaia Health, for example, analyzes recurring interactions with users to personalize physical exercises, relaxation techniques, and educational resources to the patient’s unique profile.
Challenges and ethical considerations of implementing AI in telehealth
Even in cases where the cost efficiency and potential of AI technology seem palpable, telemedicine providers shouldn’t blindly head into implementation. AI capabilities are unique, and so are their challenges. The latter, if not addressed, can cause the entire project to go off the rails.
Generalizability
You’ve probably heard about the bittersweet story of Babylon Health’s rise and fall. Once the darling of the digital care space, this telemedicine application bet big on AI for triage, claiming that its proprietary tech could diagnose patients. In the end, the company went under because Babylon Health’s AI failed where most commercial AI systems fail — it couldn’t generalize to new, diverse real-world scenarios.
If an AI model is trained on a limited number of data or homogeneous populations, it won’t be able to improve patient outcomes when faced with real-world input. To avoid Babylon Health’s scenario, healthcare organizations must diversify their training data, stress-test the model against out-of-sample and edge-case data, and evaluate it against real-world data (RWD). Involving clinicians and domain experts in testing will also help the development team uncover gaps in model reasoning.
Data privacy and HIPAA compliance
AI systems can put patient safety at risk in several ways, such as accidentally exposing data during third-party API integration or re-identifying it when linking anonymized data with public datasets. Any of these breaches would easily result in a tier 2 HIPAA violation.
The compound problem of data privacy and compliance requires a compound approach that includes:
- Implementing technical data safeguards, such as access controls, data encryption, and audit logs, to ensure data security and compliance with regulations.
- Taking care of third-party risks through zero-trust APIs, strict BAAs, and data residency rules for external vendors.
- Sticking to secure AI model development and deployment practices outlined in ISO/IEC standards and NIST AI Risk Management Framework.
- Securing explicit patient consent for data sharing, especially when a company reuses data for secondary purposes, such as AI training.
- Making human oversight and ongoing risk management a crucial part of the post-deployment strategy.
Algorithm bias
Insufficient sample sizes for certain patient groups can lead to the algorithm unfairly disadvantaging some groups over others, like missing melanoma on some skin tones. And because a development team might be focused solely on standard model performance metrics, this model bias can go unchecked until the solution is live to the end user.
To make sure the bias doesn’t creep in later in the deployment, the AI development team should:
- Analyze and characterize the data set to ensure it’s representative of racial, ethnic, and other sociodemographic groups relevant to the target patient population.
- Apply statistical methods to balance the data sets.
- See how the model performs across subgroups, rather than just aggregating overall metrics.
- Align fairness metrics with other model validation criteria.
Probabilistic nature of AI models
Some AI models, especially large language models, can perpetuate bias even when the dataset is balanced. The reason behind this type of bias lies in the model’s way of learning — it picks up the assumptions, gaps, and outdated info in the training dataset.
Also, due to the probabilistic nature of LLMs, the same prompt may get the user different answers each time. This makes model validation challenging in high-stakes clinical settings. For real-world clinical LLMs, statistical debiasing methods are in their infancy, so developers usually resort to a combination of controlled prompting, human-in-the-loop validation, and output filtering and ranking.
A more impactful approach to this solution would be using agentic, specialty-specific AI LLMs. These systems have dedicated validation layers and double-check the outputs. However, off-the-shelf LLMs like ChatGPT don’t have similar capabilities; that’s why companies need to invest more to build out such solutions and related infrastructure.
Decision-making transparency
Six in ten U.S. adults wouldn’t trust healthcare providers to diagnose diseases and develop treatment plans using AI. The pushback from patients (and medical specialists, for that matter) primarily stems from the AI’s obscure nature. AI systems recommend treatments or diagnoses based on complex algorithms that often run as black boxes — something that sets a troubling precedent in healthcare.
Here’s how providers of AI-powered telehealth solutions can make AI tools that clinicians and patients can actually trust:
- Designing AI models using Explainable AI frameworks to make sure they back up their recommendations with clear explanations.
- Involving healthcare professionals at key decision points to validate or elaborate on AI-generated recommendations.
- Allowing users (doctors and patients) to flag errors to get feedback for AI refinement.
Balancing automation with a human touch
When reliance on AI goes too far in healthcare-related applications, interactions become transactional, and patients may end up feeling like a data point. Worse, without human expertise at key moments of care, AI systems may also overlook critical care cues, such as rare conditions and emotional distress, which can only be visible to a trained human eye.
To that end, hybrid workflows — those where AI handles routine tasks and smoothly hands off emotionally sensitive interactions to a human clinician — enable telemedicine to scale personalized experiences while preserving the empathetic element of the patient experience. Developing hybrid workflows requires development teams to incorporate:
- Clear hand-off protocols that enable AI systems to accurately detect when human review is needed.
- Context-aware interfaces that notify clinicians of edge cases, anomalies, or emotionally charged interactions.
- Patient-facing transparency when users are explicitly notified of whether they’re interacting with an AI or with a human healthcare provider.
The future of AI in telehealth: upcoming trends
The virtual care interaction between the two sides of care is ceasing to be transactional, as telemedicine is shifting towards continuity and longitudinal care. To deliver on the promise of whole-person care, telemedicine needs to integrate with brick-and-mortar providers, not just as a referral endpoint, but as a core element of hybrid care models that bridge the gap between virtual and in-person care. This greater trend shapes downstream innovations in telehealth services.
Voice-first and ambient artificial intelligence
Both voice-first and ambient AI pave the way for a new era of telemedicine through natural, frictionless care experiences. Working in tandem with wearables, ambient AI can enable passive remote health monitoring, helping care providers deliver care at all times. Besides, ambient AI is good at capturing rich data, including speech, environmental sounds, patient behavior, and more, making sure physicians have a more comprehensive snapshot.
Voice-first interfaces transform routine, app-based nudges into empathetic and intuitive health check-ins, reminders, or conversational guidance — much like how a patient would talk to a human doctor.
Multi-modal AI for richer virtual exams
No matter how you slice it, virtual care visits lack the nuance of in-person care since it’s difficult to catch all the facial expressions, subtle signs, and other cues through the screen. Multi-modal artificial intelligence doesn’t default to video alone — it gathers multiple data streams, including voice tones, facial micro-expressions, wearable sensors, and more.
Together, these data streams help better simulate in-person exams and extend diagnostic capabilities for virtual care to a wider range of conditions that traditionally rely on physical presence.
Domain-specific AI models
Although medical models trained on specialty data are slowly finding their footing in healthcare, no LLM is currently authorized by the FDA and other regulatory bodies as a CDSS. It means that in modern telemedicine applications, these models are reserved for administrative, triage, or engagement purposes.
As LLMs become more clinically grounded and validated, the industry will likely see them play a significant role in supporting remote diagnostics, particularly in psychiatry, radiology, and chronic disease management, augmenting clinicians.
Agentic AI assistants in clinical workflows
Companies like Hippocratic.ai, Nabla, and Suki.ai have already paved the way for autonomous and semi-autonomous systems that can proactively handle administrative and clinical tasks. Unlike traditional, task-focused solutions, agentic AI assistants are capable of switching between tasks in a single flow.
Drawing upon generative AI, agentic AI solutions are also known for their advanced reasoning, which allows the solution to consider different options and redo steps. Due to this unique ability, agentic AI possesses the level of autonomy that enables it to proactively work alongside clinicians, documenting visits, recommending care plans, and handling follow-ups.
Integrated AI marketplaces for telehealth providers
While healthcare giants have no problem developing an AI-based solution from scratch, smaller clinics often lack the resources needed to match the industry's innovation pace. AI marketplaces would enable healthcare providers to integrate plug-and-play AI components into their telemedicine platforms.
Instead of building out capabilities from scratch, healthcare companies can shop for APIs or in-app AI services, similar to how we see healthcare companies inking partnerships with one another.
ROI of AI in telemedicine, based on our projects
For over 15 years, Orangesoft has been operating in the health technology arena, helping innovative virtual care providers develop and strengthen their unique value with the latest technology. AI-powered capabilities have always been a popular request and a common expectation in Requests for Proposal (RFP) documents.
Across our clients’ projects, we’ve seen AI deliver return on investment in multiple areas — from operational efficiency to patient satisfaction. Here are two of our projects that demonstrate the true power of artificial intelligence beyond the hype.
Our team partnered with a U.S. hospital network to scale their post-stroke patient monitoring program through a telemedicine patient app. The application incorporates wearable device integration, video assessment, personal health management, and care coordination — all enhanced with artificial intelligence:
- Predictive analytics enables care teams to identify patients at risk for complications by analyzing data from wearable devices.
- Automated triage and symptom tracking collect data from the patient before the appointment, plus allow for self-service symptom checking.
- Personalized recovery plans adjust exercises, reminders, and educational content based on patient-reported outcomes, wearable data, and recovery milestones.
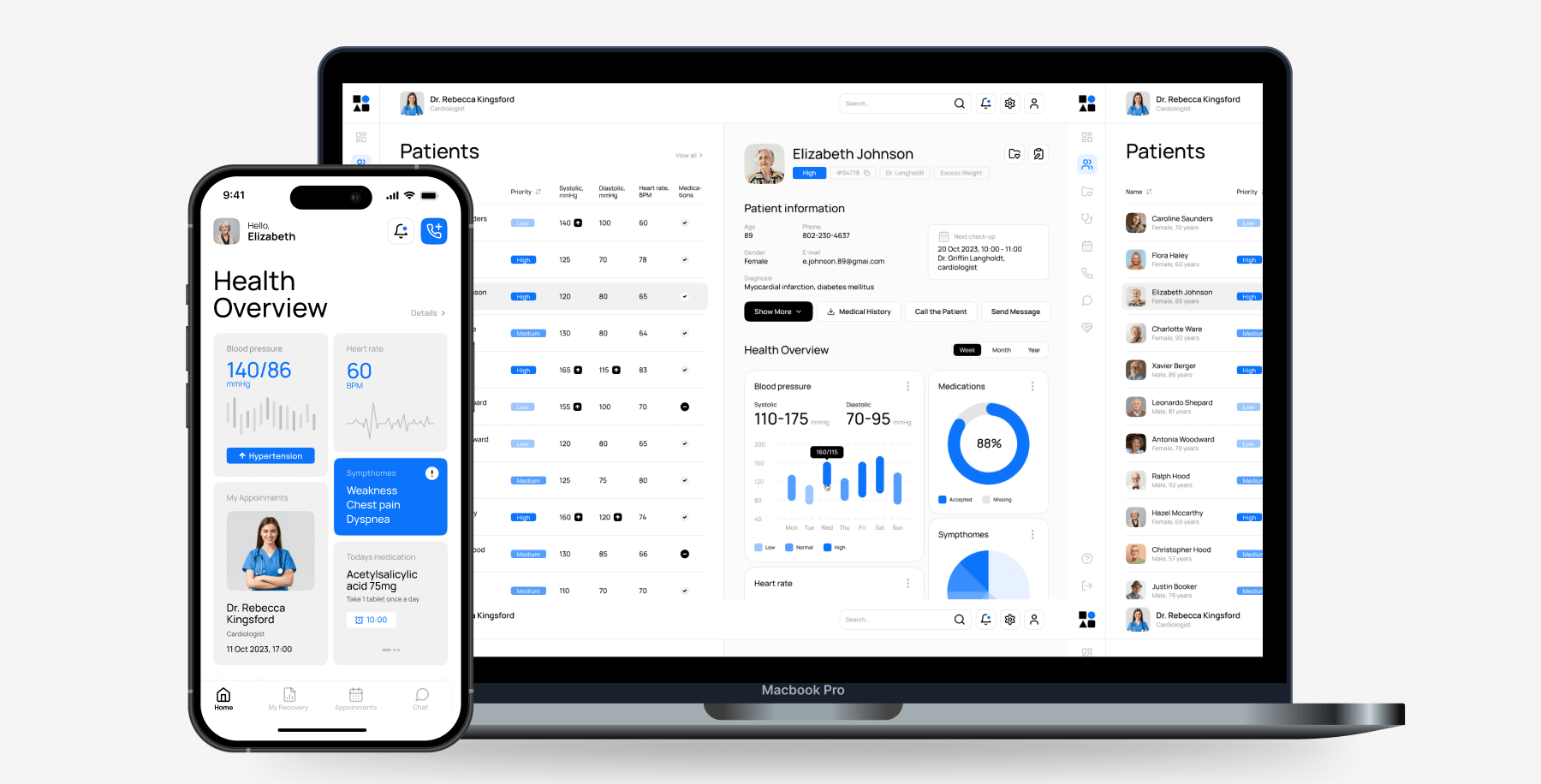
Today, the app serves over 50,000 U.S. patients, facilitating a seamless transition from hospital to home care. The ROI gains have also been impressive:
- Remote monitoring and early intervention save about ~15–25% in avoided readmission costs (for a patient base this size, it translates to around $75 million in healthcare savings annually).
- AI-powered triage and symptom tracking reduce the admin burden on care teams by 20–30%.
Smart telemedicine is no longer optional
When it comes to AI, it’s not about whether you should adopt it — it’s about nailing the use case where it can bring value for the long haul and deliver quick wins today. While mileage can vary, automated documentation, conversational AI chatbots, and AI-powered symptom checkers are among the most low-effort and quick-ROI AI innovations a telemedicine provider can adopt.
Whether you’re ready to implement one of these solutions, exploring a custom AI use case, or simply need an AI feasibility check, Orangesoft’s team can help you with any of these. We focus specifically on healthcare technology, so you can expect full compliance with HIPAA/FDA regulations, as well as IEC/ISO readiness and interoperability best practices.
