Proactive, personalized, and preventive care has long been the promised ideal for the healthcare industry. Wearable devices – capturing continuous, clinically significant data – are central to this vision. However, realizing the potential of healthcare wearables oftentimes turns out to be a challenging task. Regulatory hurdles, interoperability issues, a lack of clinical validation, and other challenges await any company venturing into wearable tech.
With 15 years of experience working with MedTech companies, we know firsthand the obvious and hidden challenges of wearable technology in healthcare. In this guide, our team offers practical insights into wearable devices and their deployment in the demanding healthcare landscape.
What is wearable technology in healthcare?
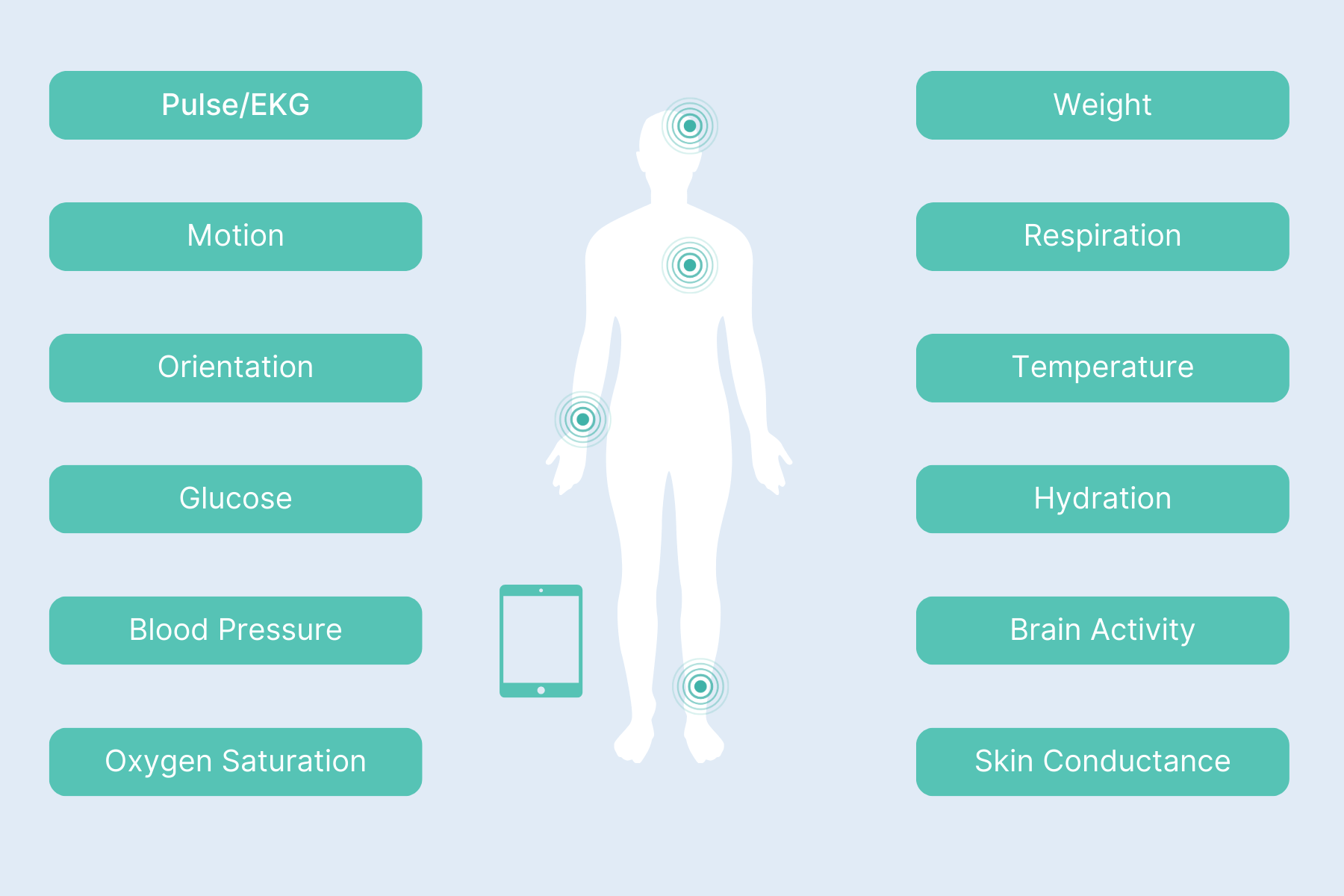
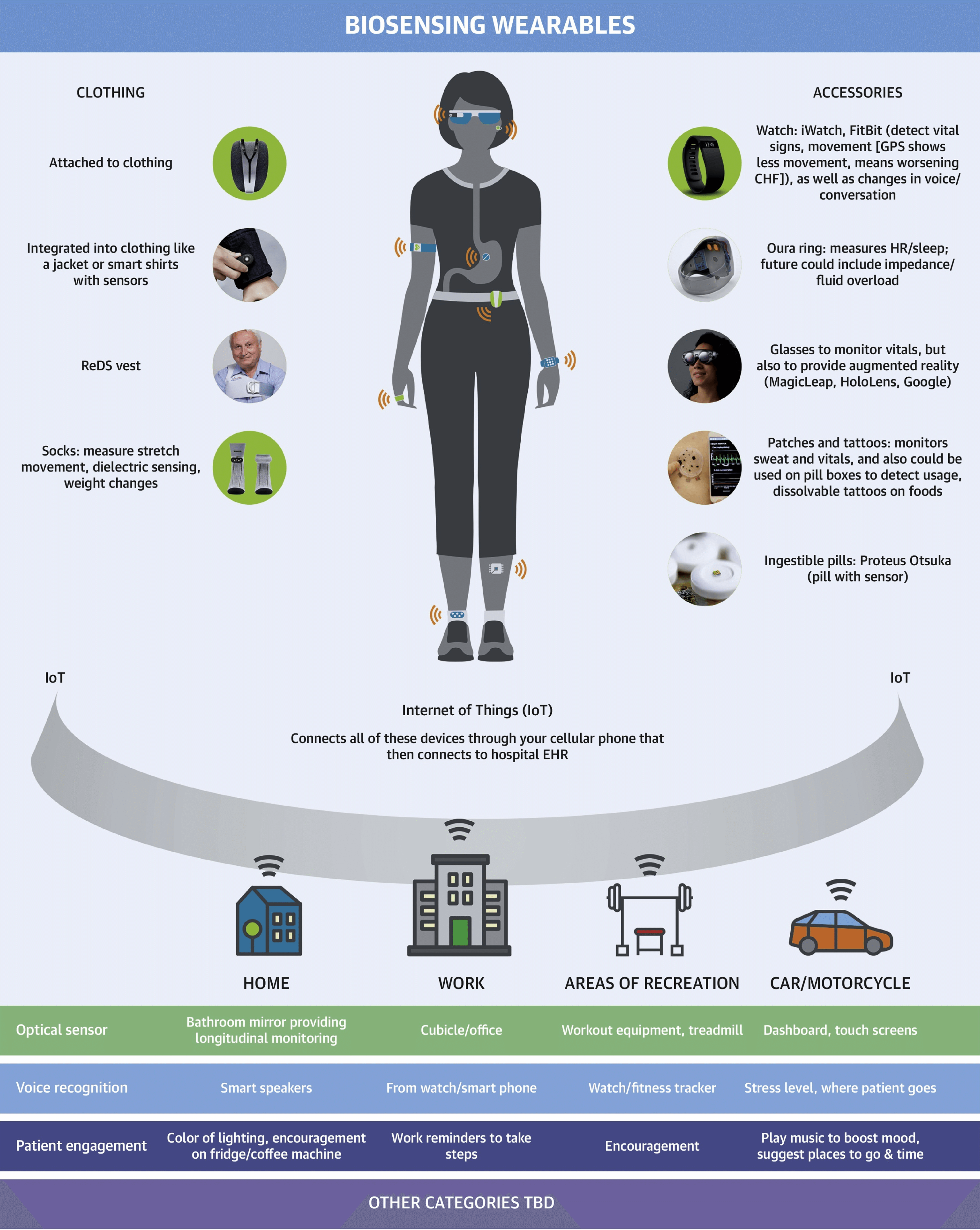
Healthcare wearable devices (HWDs) encompass a wide range of mostly non-invasive electronic devices that monitor and track various aspects of health and well-being. Usually paired with smartphones or other systems, HWDs collect, interpret, and transmit data that can be used by individuals themselves, their immediate family, healthcare providers, and researchers.
What’s particularly important for healthcare is that sensors enable a comprehensive approach to accumulating high-frequency, longitudinal, real-world data — including vital signs, speech, biofluids, retinal activity, behavioral patterns, and vibrations.
How do medical wearable devices fit into the broader healthcare tech ecosystem?
While wearable devices vary in design and data collection, they generally rely on the same Internet of Medical Things (IoMT) infrastructure to connect and share data.
It all starts with wearable data sent over to gateways, which act as the in-between layer that can manage multiple devices at once. Gateways can rely on different technologies to obtain wearable data, including Bluetooth, Wi-Fi, or cellular connections. The data is then forwarded through firewalls to the cloud server.
Being the central data hub, the cloud server houses the core data management components that process and transform wearable data into meaningful insights like personalized health recommendations. Medical staff, patients, patients’ families, and administrators can access these insights via dedicated interfaces.
In most cases, wearable data is integrated straight into electronic health records to give clinicians a more complete picture of a patient’s health — as opposed to episodic care.
Types of wearables in healthcare, by end-user
Healthcare wearable devices can be divided into consumer-grade wearables and medical-grade wearables.
Consumer-grade wearables
Consumer-grade wearables such as smartwatches and fitness trackers are traditionally considered to be less accurate and to have a wellness, not medical, focus. Usually, non-prescription, consumer health-related devices have a much lighter compliance burden compared to medical devices.
But as patient care extends beyond hospital walls, consumer-grade wearables are increasingly being used for medical purposes, and vice versa. For example, in 2024, the FDA cleared the first over-the-counter continuous glucose monitoring patches, allowing individuals to buy a CGM without the involvement of a healthcare provider.
Medical wearable devices
Medical-grade wearables are usually the ones integrated into the larger healthcare tech ecosystem, providing accurate data for clinical decision-making, disease management, and remote patient monitoring. Because they're designed for medical use, these devices are subject to regulations, such as those enforced by the FDA in the United States.
Types of medical wearable devices, by function
Today, there are approximately 2 million different kinds of medical devices on the global healthcare market that fall into over 7,000 generic device groups. Let’s overview the most popular types of healthcare wearable devices, divided by function.
Health monitoring
Health monitoring devices are exactly what the name implies: they are used to monitor health within and beyond healthcare settings over time, often continuously or at regular intervals. Healthcare providers can draw on the continuous stream of data these devices provide to:
- Monitor vital signs of at-risk and chronic patients (patients with heart diseases, diabetes, hypertension, sleep apnea, etc.)
- Keep tabs on the patient’s activity and mobility levels.
- Monitor physiological indicators of stress to inform stress management strategies.
- Support remote patient monitoring programs and telehealth offerings.
- Adjust treatment plans and recommendations based on longitudinal data.
- Advance medical research and collect more data for the development of algorithms and predictive models for disease prediction and prevention.
- Obtain real-time data from participants in clinical trials.
If processed with prediction modules, data from health monitoring sensors can be used to predict the likelihood of diseases or future episodes.
For individuals, health monitoring devices serve as a source of insights that can inform lifestyle changes and put them in the driver’s seat of their health and well-being.
Examples of health monitoring wearable devices: ESGs, blood pressure monitors, CGMs, EMGs, e-skin patches, wearable sensors for specific biomarkers, smart socks, wearable bio-fluidic patches, sweat sensors, and more.
Screening
Screening medical wearable devices help healthcare professionals spot potential health issues — before they become serious — and decide whether they need to proceed with specific diagnostic testing for a given patient.
Common use cases for screening wearable devices in healthcare include:
- Tracking sleep patterns and breathing irregularities to identify sleep disorders.
- Screening cardiovascular risk patients for heart rhythm abnormalities.
- Tracking glucose trends over time to identify patients with undiagnosed prediabetes or type 2 diabetes.
- Tracking movement and walking patterns to identify patients at risk for falls and more.
Examples of medical wearables for health screening: gait sensors, sleep apnea monitors, ECG monitors, CGMs, wearable ultrasound patches for breast cancer screening, and more.
Patient therapy or drug delivery
Medical wearables can also help healthcare providers administer treatments or medication directly to patients. Patient therapy or drug delivery wearables can react to changes in real-time data to deliver medications or treatments — or act based on pre-programmed schedules.
Drug delivery wearables can become a springboard to:
- Ensuring dosing accuracy for diabetes patients.
- Treating conditions like chronic pain, epilepsy, Parkinson's disease, and essential tremor (e.g., delivering electrical stimulation to specific areas of the brain or nervous system).
- Supporting personalized treatment strategies (e.g., adjusting medication dosages based on real-time physiological data).
Patient therapy delivery wearables help deliver non-pharmaceutical therapies remotely, activating natural pain relief mechanisms or providing sensory input to modulate specific functions.
Use cases for such HWDs include:
- Electrical stimulation for pain management
- Light/heat therapy for skin conditions
- Sound therapy for tinnitus or sleep disorders
- Biofeedback for stress management or pelvic floor strengthening
Examples of patient therapy/drug delivery wearables: CGMs integrated with insulin pumps, infusion pumps, non-invasive drug delivery patches, microneedles, wearable injectors, photobiomodulation (PBM) devices, implanted pacemakers, and more.
Patient rehabilitation
Rehabilitation activities are an iterative process that necessitates continuous assessment of the recovery progress and specialized rehabilitation training. Whether inside or outside medical facilities, biofeedback is a valuable tool to monitor the physiological activity of the human body and obtain a more detailed evaluation of the impairment.
Medical wearables can capture real-time biofeedback so that physicians and therapists can tailor rehabilitation therapies to maximize recovery, while patients can draw on that data to self-manage rehabilitation progress.
Medical wearables for rehabilitation aid in:
- Tracking energy expenditure among cardiac rehabilitation patients to assess the effects of medications like beta-blockers.
- Assessing movement patterns to identify imbalances that might be the cause of pain or instability for patients with musculoskeletal conditions.
- Rebuilding muscle strength after injury or surgery through electrical stimulation.
- Supporting patients with weakness or paralysis due to neurological conditions, such as ALD, ALS, and others.
Examples of patient rehabilitation wearables include: smart gloves, FES systems, motion sensors, IMUs, sEMG, prosthetic limbs, exoskeletons, conductive elastomers, and others.
| Anatomy | Device type | Environment data | Performance data | |
| Raw data | Application format | |||
| Head | Glasses | Blind spots | Eye movements | Fatigue/Concentration |
| Augmented reality glasses | Integration of digital worlds with reality (layering) | Body movements, eye movements, facial expressions | Emotions, mental states, physical condition | |
| Wrist | Wristbands | Air temperature, humidity, pressure, GPS, sound/noise, light | Body movements | Physical condition (overall health, analysis of endurance), energy expenditures (calories), group dynamics (geographical proximity between employees), productivity (speed of movements) |
| Body temperature | Physical condition (overall health), emotions (arousal) | |||
| Blood oxygen saturation, blood pressure | Physical condition (analysis of endurance) | |||
| Heart rate variability/blood volume pulse | Emotions (valence and arousal), productivity | |||
| Electrodermal activity | Emotions (arousal) | |||
| Chest | Bra | n/a | Circadian metabolic changes in heat | Cancer prevention |
| Fingernail | Patch | Ultraviolet rays | No data collected | No data collected |
| Feet | Soles | GPS | Body movements | Physical condition (overall health, analysis of endurance), energy expenditures (calories) |
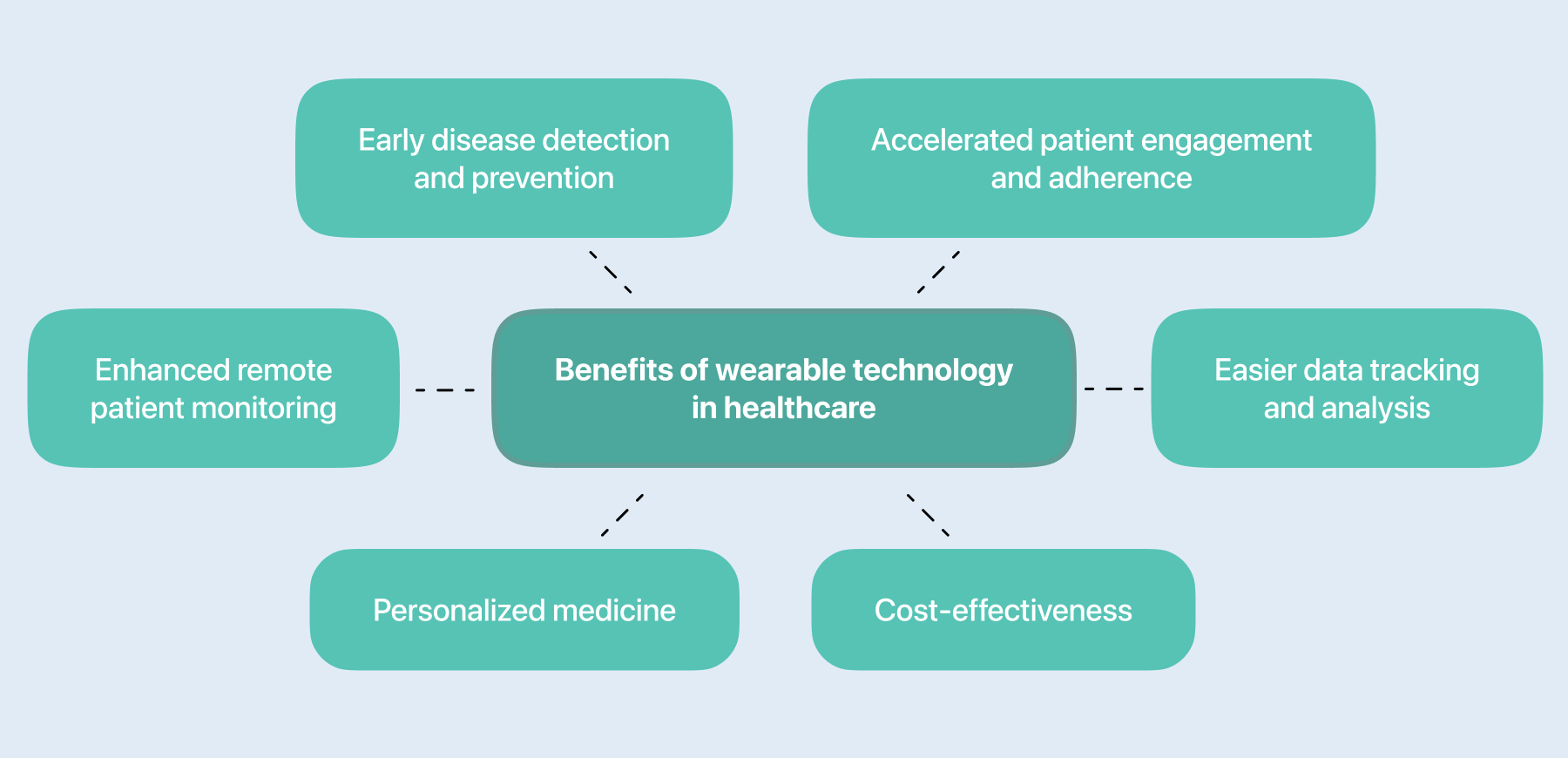
Benefits of wearable technology in healthcare
In 2024, the global wearable healthcare devices market stood at over $30 billion. By 2029, it’s projected to grow to over $76 billion, driven by the shift to remote care models, the imperative to optimize healthcare costs, and the promise of personalized medicine.
Enhanced remote patient monitoring
The traditional clinical care model hinges on episodic encounters between patients and healthcare providers, which inherently limits data collection capabilities. Plus, a significant portion of care for chronic, cancer and other long-term illnesses happens at home, where patients are one-on-one with complex decisions, like “What do I do when my condition worsens?”
Blood pressure cuffs, glucometers, ECGs, and other remote monitoring wearables enable continuous data collection of patients’ symptoms and other health-related outcomes within ambulatory settings and at home. For care teams, this health data can inform treatment plans and medication adjustments, enable early detection of health implications, and facilitate timely interventions based on alerts.
RPM systems, enhanced with wearable technologies, allow 38% of RPM users to prevent readmissions for chronic patients and reduce the cost of chronic care by 17%.
Early disease detection and prevention
Consider this: over 80% of cardiovascular disease deaths are preventable. Wearable technology emerges as a game-changing ally in this fight. Medical sensors offer deeper, real-time, longitudinal insights into health metrics that — when integrated with medical records — enable doctors to detect early signs of disease and prevent it from progressing.
By collecting more data points, HWDs also allow healthcare teams to bypass the limitations of traditional protocols that often rely on occasional checks, thus missing important variations in health metrics.
Personalized medicine
Only 40% of factors that influence our health have to do with genetics and medical history. Sadly, the other 60%, which include our lifestyle, nutrition, and the environment, have not been traditionally factored into medical recommendations. Medical wearables can monitor data across the board, whether it’s environmental data, sleep, steps, or any other metrics, to inform tailored healthcare interventions based on individual variations.
Accelerated patient engagement and adherence
Wearable-based self-monitoring allows patients to take a more active role in their health management and improve their awareness of key health metrics. Those who actively track their health data and send these insights over to providers are also likely to have better health outcomes.
Thanks to routine tracking, providers can monitor the patient’s adherence to prescribed treatments, exercise regimens, and lifestyle recommendations. For example, smart pill bottles — that track pill bottle openings — can improve medication adherence and alert healthcare providers or caregivers if a dose has been missed.
Cost-effectiveness
Currently, around 50% of the U.S. population has a chronic disease, with 86% of all healthcare costs attributable to chronic disease management. Data collected by HWDs enriches a doctor’s understanding of a patient’s health, allowing healthcare professionals to spot subtle changes in vital signs long before they become serious health events.
This proactive approach from the provider’s side, along with better self-management options for patients, eases the burden on secondary care services and prevents costly hospitalizations. Also, wearables proved effective in reducing care delivery costs. For example, cardiac monitoring patches are 90% cheaper to identify arrhythmias compared with an implantable loop recorder.
Easier data tracking and analysis
One of the drawbacks of traditional ambulatory devices is their intermittency, meaning they collect data at pre-determined intervals or need an external trigger to do it. As we’ve already mentioned, wearable devices are always on, allowing care teams and individuals to pick up fluctuations and trends that would otherwise be missed. Also, HWDs can collect multiple metrics at once.
Instead of on-device storage typical for traditional ambulatory devices, medical wearables send data in standardized formats to cloud platforms, making it easier to store and use the data for ML model training.
Key roadblocks on the way to adopting wearable health technology
As a crucial enabler of continuous health monitoring and proactive care, medical wearable devices hold immense transformative promise in healthcare. However, to succeed in the medical wearable technology market, medtech companies and device manufacturers first need to clear a number of hurdles.
Data accuracy and reliability
The reliability and accuracy of wearable data is one of the tension points that can impede the proliferation of the technology in the field. Wearable devices, including medical-grade ones, may be susceptible to factors such as sweat, skin contact, and others that can introduce noise into the data. Then, there are noisy wireless and electromagnetic environments that can result in Radio Frequency Interference and data transmission errors.
If the device drains the battery too quickly, it means that it may sacrifice the sensor sampling rate and the processing power to mitigate the battery depletion.
To battle the challenges we’ve mentioned above, it’s important that companies:
- Lay advanced device design at the core of their solutions (e.g., microfluidics, advanced optical sensors) or design the hardware in a way that makes it less sensitive to environmental factors.
- Employ advanced battery tests, emulation software, and battery drain analysis to understand the profiles of actual batteries.
- Adopt a broad approach to calibration and validation of wearables to make sure they capture the necessary nuances and variations.
- Use advanced algorithms for noise reduction and signal filtering.
- Leverage ML models that can recognize and compensate for noise patterns and missing health data.
Regulatory compliance
Medical-grade wearables have a direct impact on an individual’s health and safety, which makes them fall within the stringent regulatory landscape. Regulations vary by country. In the US, medical devices are regulated by the FDA and can be classified as “FDA Registered,” “FDA Cleared,” or “FDA Approved” based on their risk class and additional requirements.
In the EU, HWDs fall under the scope of Medical Device Regulation (MDR) 2017/745, which categorizes wearables into four classes based on their risk and intended purpose.
What’s common for all regulations is their emphasis on the safety and high performance of devices that are ensured through clinical evidence. To plan for successful market entry, companies must implement a comprehensive regulatory framework from the initial product development stages.
The regulatory framework includes a robust quality management system based on ISO 13485, a risk management strategy, and a data security framework in line with applicable data privacy regulations (HIPAA, HITECH, GDPR) and industry standards.
Interoperability and integration issues
Unless designed for tech and data interoperability, HWDs have a hard time integrating with other healthcare systems and other health data sources. Inconsistent data formats, proprietary communication protocols, and a lack of standardized APIs are some of the underlying causes for the low level of interoperability.
Not only does the lack of interoperability drive a fragmented view of patient health, but it also limits the potential for AI-based analytics and predictive modeling that thrive on consolidated and standardized data.
To tackle the interoperability barrier, device manufacturers should:
- Adopt open data standards such as FHIR and HL7v2.
- Implement automated software testing to check the APIs for health system integration, validate data formats, and ensure protocol compliance.
- Employ data mapping and transformation tools to account for differences in data definitions and ensure accurate interpretation.
Security and data privacy risks
While 91% of patients are interested in sharing their wearable health data with healthcare providers, the other 9% are wary of that because of the potential security risks. Those 9% are not wrong: the IoMT ecosystem is full of inherent vulnerabilities present on every exposed network interface, including Wi-Fi and Bluetooth.
Also, wearable health data is time-stamped and quite detailed, which automatically increases the risks of re-identification. Even the robust traditional de-anonymization techniques aren’t able to guard the data from ML-based reverse anonymization that’s often used by malicious actors.
To protect the data received and transmitted, we recommend companies to adopt the following security measures:
- A multi-layered approach to data security that spans both the tech aspect, governance, and ethical considerations.
- Stringent access controls, end-to-end data encryption, regular security audits, penetration testing, and more.
- Advanced data minimization and anonymization techniques, including differential privacy, federated learning, K-anonymity, and others.
User adoption barriers
Today, around 44% of Americans own wearable devices, which is impressive but still far from wide adoption. Several factors slow down the widespread integration of HWDs into the lives of healthcare consumers. Some wearable systems may not be age-friendly or accessible enough for some patient categories to get their heads around.
In some cases, user adoption is dampened because of insufficient internet connectivity, especially in rural areas. Socioeconomic factors also play a significant role, with the high cost of wearables being a turn-off to many individuals.
Although wearable device manufacturers cannot eliminate all barriers single-handedly, they can at least do what’s in their responsibility area to sustain HWD usage:
- Focus on human-centered design that’s mindful of the diverse range of user capabilities and desired outcomes.
- Include users in your design planning and draw upon their feedback to iterate the software designs.
- Provide comprehensive user education and support, including exhaustive instructions, troubleshooting resources, and tailored assistance.
- Adjust software and algorithms to minimize hardware requirements and reduce the complexity of devices.
- Offer a range of price points through tiered product lines.
How to integrate healthcare wearables with IoMT platforms
HWDs can’t exist in a vacuum or in a silo. To live to their fullest potential, they need to integrate into broader IoMT platforms of an EHR vendor, a specific hospital, or an RPM program. Here’s how you can make this integration as smooth as possible.
Step 1: Analyze platform compatibility
First, device manufacturers need to gain clarity on the APIs, data formats, and communication protocols used by the target platforms. Interoperability requirements, including data types, formats, and transmission protocols, are also something to account for if they design for a seamless data exchange.
Even if the wearable device is developed with regulatory compliance in mind, the regulatory requirements for integration might be different. That’s why it’s important to check the specific cybersecurity regulations, data security regulations, and IT practices.
Step 2: API integration and data mapping
To make the wearable device and the IoMT platform speak the same language, device companies need to develop API integration modules that can translate the wearable data and send it to the IoMT platform's API. For example, if the IoMT platform relies on a REST API, developers create modules that make HTTP requests (GET, POST, PUT, DELETE).
Next goes data mapping and transformation tools that make sure no data is misinterpreted or lost during transfer. Data mapping and transformation solutions also align data formats between systems for accurate storage and data display in the IoMT platform.
Say your wearable is a heart rate monitor that makes measurements in beats per minute (BPM), while the target IoMT platform stores it as a numerical value with a specific unit code. A data mapping tool is what would transform the wearable's BPM data into the platform's numerical representation.
But however robust and advanced API integration modules and data mapping techniques are, no system is immune to data exchange failures. This makes effective error-handling mechanisms an indispensable safe net for the integration to sort out data errors and exceptions.
Step 3: Take care of data security and privacy compliance
The security of the integration is another quite resource-intensive yet salient effort that requires a systemic approach, including:
- End-to-end encryption for data transmitted between the wearable device and the IoMT platforms.
- Robust access controls to make sure only authorized users and systems can get their hands on the data.
- Privacy compliance with applicable regulations, such as GDPR, HIPAA, and others, and the privacy policies of the IoMT platform.
- Continuous security testing to nip potential integration vulnerabilities in the bud.
Step 4: Test and validate
The final stretch of the integration is end-to-end testing paired with usability and performance tests. Together, these will validate the system through and through, de-risking it for end users and making sure all components work as intended and in sync. Clinical validation is another approach that can help assess the system's accuracy and reliability in a clinical setting — and obtain real‐world evidence for regulatory approvals.
Step 5: Deployment and continuous monitoring
When it comes to deployment, we recommend starting small by making the integration available to a small group of patients first. A soft launch gives providers more maneuver to make adjustments based on patient feedback and then gradually expand deployment to a broader user base.
Post-deployment, healthcare providers and patients require training and support to successfully adopt the solution and operate it effectively. Also, the entire system requires a vigilant, ever-present watch to swiftly address any performance issues that occur down the road. To truly unlock the system's potential, IoMT platform providers can also implement analytics tools to transform the treasure trove of wearable data into actionable reports and dashboards.
Wearable AI, the best of both worlds brought together
Traditionally, wearable data is handed over to a separate system, like a cloud server or an app, for analysis and insights generation. However, this back-and-forth may result in slower data processing and higher latency, which, considering the stakes involved, can potentially compromise patient safety.
Wearable AI eliminates the lag in data processing by having algorithms integrated right at the core of the wearable devices. Although this concept hasn't really caught on yet, wearable AI is poised to overcome the limitations of the current approach to wearable data analytics. Our AI team has curated the main differences between the two approaches below.
| Feature | Wearable AI | Traditional approach (Wearables + AI models + analytics) |
|---|---|---|
| Data processing location | On the wearable device or very close to it (edge computing) | In a separate location (cloud server, mobile app) |
| Real-time processing | Yes | Often delayed |
| Latency | Minimal latency, allows for immediate feedback or interventions | Higher latency due to data transmission and processing time |
| Connectivity requirements | More autonomous, can function even without a constant internet connection | Hinges on a stable internet connection to transmit and analyze data |
| Data flow | Data analysis happens locally → insights provided in real-time | Wearable collects raw data → data is sent to an external system → AI models analyze data → results sent back to the user |
| Example | Wearable ECG monitor with embedded AI detects irregular heartbeat and triggers instant alert | Wearable ECG monitor records the heart's rhythm data, and transmits it wirelessly to a smartphone app. The app then analyzes the data with cloud-based AI algorithms. If arrhythmias are detected, the app sends an alert to the user's smartphone and their healthcare provider |
Future trends for wearable technology in healthcare
If there’s one thing we’re positive about, it’s that wearables, both medical-grade and consumer-focused, will continue permeating the healthcare industry, ushering in new modes of care, new modalities of patient engagement, and a paradigm shift towards proactive health management. Let’s see what the future holds for wearables.
Smart tattoos and e-skin
Tattoos, erstwhile solely a body art, are making their way into functional healthcare wearables. Smart tattoo pigments, applied under or onto the skin, can track vital signs, deliver medications, and monitor muscle signals. What drives this concept is that smart tattoos can’t be hacked or run out of battery, which, paired with low fabrication costs, makes them an increasingly attractive option for continuous health monitoring. To date, the technology is still under testing and will undergo human clinical trials in the coming years.
Another anticipated dermal modality of wearables is e-skin, which consists of soft and stretchable material with nerve-like electronics. The technology is expected to upgrade modern prosthetics by providing a sense of proprioception, enhancing the user's ability to feel the world around them.
Smart clothing
In 2024, the smart clothing market, which includes e-textiles, smart wear, and smart fabrics, was valued at $5.16 billion. From 2025 to 2030, it’s expected to leap at a CAGR of 26.2%, driven by its potential to provide long-term, unobtrusive methods for cardiac, respiratory, and activity monitoring, especially for older patients.
So far, smart gloves have found particular traction in rehabilitation and sports training, but the development and successful adoption of other smart clothing depends on flexible and stretchable sensors that would make wearable garments comfortable, durable, and seamlessly integrated into the patient’s life.
Wearable neurotech
Non-invasive neurotech is another trend slated to advance in the coming years. These therapeutic medical devices, usually in the form of head-mounted wearables, can deliver brain stimulation non-invasively through the skin and skull to treat various chronic health issues. These wearables will help individuals self-administer alternative treatments for depression, PMS, anxiety, and many other conditions that don’t always respond well to drugs.
The market for wearable neurotech is still modest, with a few FDA-cleared products. But we can expect its rapid growth as long-term R&D is transitioning into commercial products that are pending regulatory approvals.
Medical wearables for women
By 2033, the women’s health market is expected to grow to $59.5 billion, an impressive increase from $42.57 billion in 2024. This market expansion puts the gaps in women’s health on a sharp display, including the lack of methods to timely diagnose and support conditions like PCOS, menopause, perimenopause, and others.
Wearables can catch up to women’s unique needs, as demonstrated by the statistics: around 85% of women are willing to use wearables to better understand their bodies, while 75% would also use them to improve their health. Healthcare wearables can track long-ignored data such as hormonal fluctuations, menstrual flow volume, pelvic floor muscle activity, and more, transforming female healthcare for generations to come.
Seize the accelerating market of medical wearables with Orangesoft
The future of personalized healthcare is connected, and it’s accelerating. But to capitalize on the exciting opportunities of healthcare wearables, you need to get all the puzzle pieces right. From robust data management to compliance and easily scalable architecture, Orangesoft will help you address the complexities of healthcare wearables — not just from the tech perspective but also from a strategic and user-centric standpoint.
