Back in the day, patients diagnosed with chronic conditions had to grapple with frequent hospital visits. Today, remote patient monitoring (RPM) software enables high-risk patients to receive care from the comfort of their homes. As a revolutionary care modality, remote patient monitoring systems also enable real-time assessment of a patient’s well-being, empowering healthcare providers to remotely manage patients requiring chronic, post-discharge, or senior care.
However, the development of RPM systems is peppered with challenges, including technical and non-technical hurdles. So, let’s broach the subject and look into the potential, challenges, and development workflow of a remote patient monitoring platform.
Benefits of developing remote patient monitoring software
In 2023, over 81% of clinicians used RPM on patients — a 305% increase compared to 20% in 2021. The adoption of RPM tools — ranging from wearables to more sophisticated devices such as pulse oximeters and ECG monitors — is increasing due to a range of factors that benefit both patients and healthcare providers.
Improved access to care
RPM systems expand access to care by bringing it directly to patients, wherever they are. This improved accessibility is beneficial for patients in remote areas or those with limited mobility. In urban and rural areas, 65% of doctors have adopted remote patient monitoring for medical management.
Remote patient monitoring apps also provide a vital lifeline for at-risk populations, allowing older adults and immunocompromised individuals to manage their health conditions without leaving their homes.
Early detection of health issues
By regularly tracking health metrics, RPM tools enable healthcare providers to intervene earlier if a patient shows signs of deterioration. Earlier detection of changes in a patient’s health status also leads to fewer implications and better patient outcomes. For example, AI-enabled monitoring tools that process patient health data can alert care groups when a diabetic patient has dangerously high blood sugar levels.
Reduced readmissions
Early detection prevents minor issues from becoming emergencies and hospitalizations, keeping more beds available. Remote monitoring technology also allows for earlier discharges as doctors can keep a watchful eye on recovering patients remotely. The University of Pittsburgh Medical Center, for example, reduced the risk of hospital readmissions by 76% by providing patients with tablets and RPM equipment.
Personalization of care
By analyzing patient-generated health data and integrating it with the electronic health record, medical providers can make targeted adjustments to medication dosages, treatment protocols, or lifestyle recommendations. For example, having a personalized medicine approach in a long-term care center enables the care team to make quicker decisions about treatment, such as adjusting rehabilitation regimens.
Enhanced chronic disease management
Managing chronic diseases requires a multifaceted approach that relies on strong coordination within care teams and strong rapport between patients and providers. Seamless sharing of vitals, medication adherence data, and other patient information between patients, HCPs, and specialists promotes a more collaborative approach to care and allows for monitoring of a patient's progress between in-person visits.
Reduced healthcare costs
Remote monitoring tech can not only save lives, but also money. Over the next 25 years, RPM is expected to save $200 billion in healthcare costs globally across all conditions. The technology contributes to savings in many ways, including earlier interventions, lower hospital readmission rates, more effective chronic disease management, and reduced doctors’ workloads.
Increased patient engagement and satisfaction
40% of people living with long-term conditions want to be more involved in their health management. RPM tools can be effective by placing crucial health data at patients’ fingertips and giving them more control over their well-being. By making it simpler for patients to participate in treatment, RPM platforms improve medication adherence, promote healthier lifestyle choices, and instill a greater sense of patient ownership over their health journey.
Optimized resource allocation
By automating data collection and analysis, remote patient monitoring systems eliminate the need for manual data entry, leaving providers more time for critical tasks. Hospital-at-home initiatives, backed up by RPM, help prioritize high-touch, in-person resources for providers and focus attention on patients who require immediate intervention.
101 on remote patient monitoring system architecture
The architecture of a remote health monitoring system is multi-layered, comprising five core components that enable uninterrupted data flows within the system.
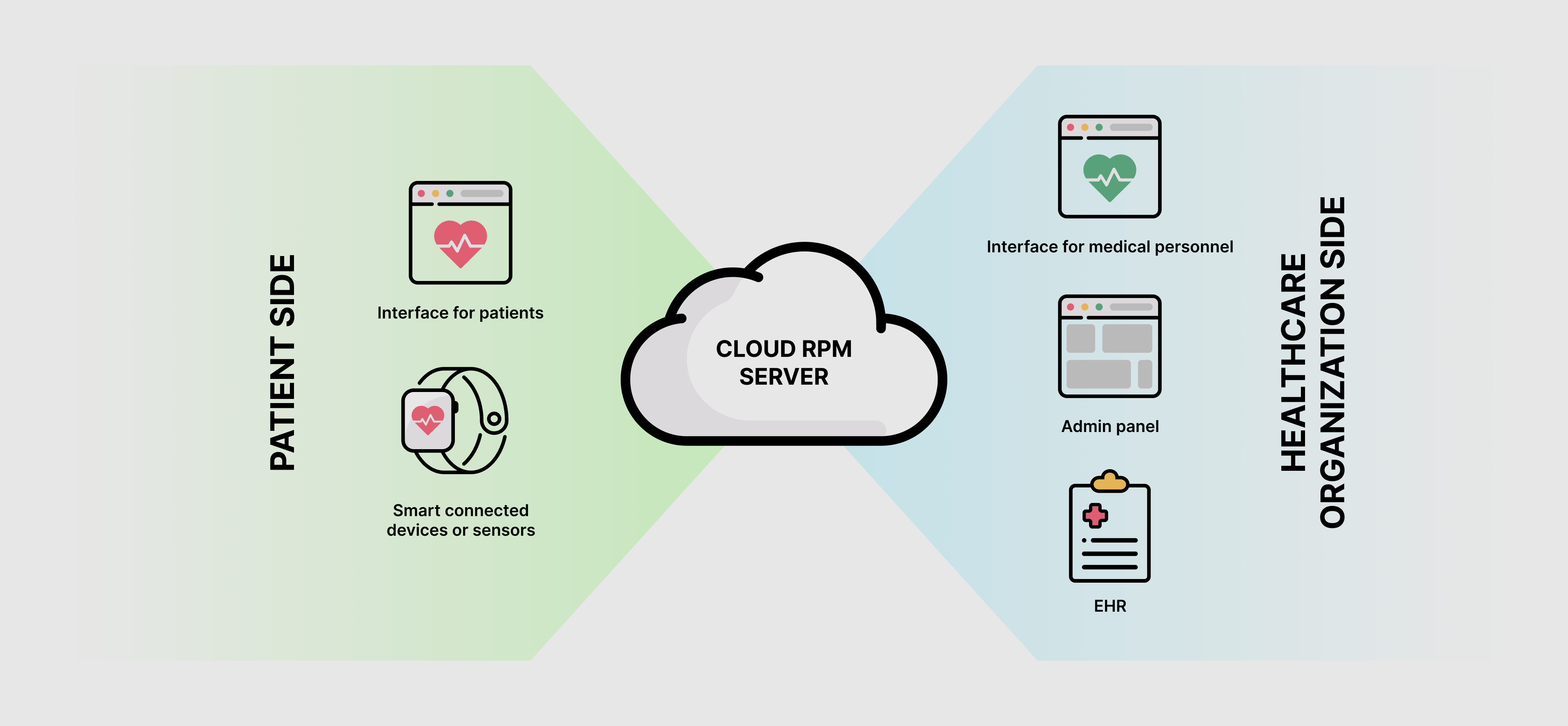
Smart connected devices or sensors for patient monitoring
Remote monitoring devices, including EKG/ECG monitors, sleep trackers, smartwatches, blood pressure monitors, and other wireless hardware, constitute the sensor layer of the architecture. They collect (and sometimes store) specific health data, including vital signs, weight, and blood pressure, and then transmit this data to the dedicated mobile app via Bluetooth or directly to the cloud via the Internet.
Patient interface
Patient-facing RPM apps team up with medical devices to collect real-time health data. The app also provides an interface for manual data input, allowing patients to log their symptoms and medication intake.
Remote patient monitoring apps are typically augmented with visualizations that enable patients to track their health trends over time. Such apps can also leverage telemedicine capabilities, providing videoconferencing tools for appointments, follow-ups, medication prescribing, and virtual consultations.
Cloud RPM server
At the heart of the RPM system is the storage and processing engine, which is usually a collection of cloud services that securely record, process, and analyze device data, as well as data from the RPM app. The RPM server also integrates with an EHR system to source PHI in FHIR format and spot trends in patient data, such as early signs of complications.
Medical staff interface
The medical staff interface has a bi-directional connection with the cloud RPM server. The interface typically includes several built-in modules that enable care teams to effectively manage and act on patient data.
- Data visualization module. The module delivers a 360-degree patient view to the provider, supported by charts and graphs that visualize trends in vital signs, medication adherence, or other relevant data points.
- Alert management module. The module enables alerts generated by the system when predefined thresholds are met or exceeded. Clinicians can receive notifications for critical situations via SMS, email, or in-app notification. The system can also warn about device failures in real time.
- Reporting module. By generating custom reports on patient data, the module helps deepen insight and track progress over time.
- Communication module. This module, made of two-way messaging, video chat functionalities, and/or telephony integration, is responsible for secure, remote communication between clinicians and patients.
- Appointment management module. This module is used to store patients’ appointment details and manage patient-provider interactions. Usually, this module allows for two-way scheduling, enabling both patients and doctors to initiate appointment requests.
Depending on the organization's unique needs, a doctor-facing RPM interface may also include modules for patient management, care plan management, and patient education.
Admin web panel
The RPM architecture also relies on a control dashboard that empowers administrators to configure roles and access permissions, add new patients, set alarm parameters, and perform other activities related to the behind-the-scenes operations of the RPM system.
Key features of a remote patient monitoring solution
Developing RPM solutions isn't just about creating a software product; it's about creating a positive impact on people's lives. To embrace its crucial role in the system, a remote patient monitoring application should be geared up with six core features.
Real-time patient health tracking
To enable instant capture of a patient’s health status, your RPM system should be able to retrieve health data from medical devices in real-time or at predefined intervals. The interplay of wearable sensors, wireless communication, IoT, and cloud computing allows for continuous health monitoring, where:
- The IoT ecosystem enables the integration of an RPM solution with multiple health-tracking devices for the seamless exchange of data between patients and providers.
- Wearables collect and wirelessly transmit data to a central system.
- A secure cloud platform stores, analyzes, and sends processed health data to medical professionals for further review.
Data analytics and reporting
An ideal RPM technology enables care teams to not only monitor patient health metrics but also interpret physiological data. Data analytics, enabled by machine learning algorithms and joined by data visualization tools, transforms raw patient data into a dynamic wellspring of actionable insights. This real-time intelligence empowers healthcare providers with the following capabilities:
- Analysis of patient vital signs against preset thresholds.
- Early detection of potential health problems or worsening conditions.
- Risk alerts on biometric data, symptom surveys, activity, medication adherence, and more (for example, when heart rate and systolic blood pressure exceed the acceptable ranges).
- Breakdown of historical trends in the patient's data to identify unusual fluctuations.
- An integrated dashboard of patient health data, with a rating/severity score for each patient.
- Automated generation of monthly reports based on patients’ vital data and more.
By interpreting and visualizing data, this capability of RPM systems promotes proactive care strategies and optimizes workflows, ultimately fostering better care outcomes and a more efficient healthcare system.
IoT-based monitoring of RPM devices
Integrating an RPM system with multiple medical devices enables combined data insights and data correlation analysis that would otherwise be impossible. For example, by integrating a smartwatch for heart rate and activity tracking with a blood pressure cuff and a glucometer, a remote monitoring system enables a broader scope of remote diabetes management.
IoT-based monitoring of RPM devices also facilitates easier configuration of RPM parameters and identification of device failures.
Accessibility features
Accessibility is another important consideration for an RPM app, ensuring that everyone has the opportunity to benefit from the technology. To cater to all patient groups, your RPM platform should incorporate the following accessibility features:
- Voice control for data entry or navigation to facilitate adoption among patients with visual impairments and motor dysfunctions.
- Text-to-speech functionality to improve content accessibility to those with visual impairments, dyslexia, and other disabilities.
- Patient-first, accessible design that includes screen reader compatibility, high-contrast mode, clear interface elements, support of multiple languages, and more.
Overall, the system should be developed with non-tech-savvy user groups in mind and take into consideration the accessibility design guidelines such as WCAG and CVAA.
Patient-doctor online communication
Both remote patient management and telemedicine are fundamental components of virtual care, reinforcing each other’s impact. Integrating an RPM solution with a telemedicine platform, or augmenting it with telemedicine capabilities, provides the foundation for two-way communication between parties, enabling proactive outreach to patients and continuous remote care.
Here are some key telemedicine functionalities an RPM system can build on:
- Secure video conferencing is used for virtual consultations to conduct check-ins, discuss treatment plans, and monitor patients' conditions visually.
- Secure messaging to schedule follow-up appointments, send/get updates on the patient’s condition, and adjust treatment plans.
- A library of educational resources, including FAQs, a video library, exercise tips, and more, tailored to specific health conditions.
- Patient engagement tools, such as appointment reminders, medication adherence trackers, or educational quizzes.
- Remote prescription management to eliminate the need for in-person visits.
Remote patient monitoring system development process in 6 steps
Once you have a solid grasp of your software product idea, you can turn to an experienced software development company to implement your vision. When contacting your tech partner, you don’t need to have detailed software requirements ready — a high-level understanding of functionalities is enough to get the ball rolling.
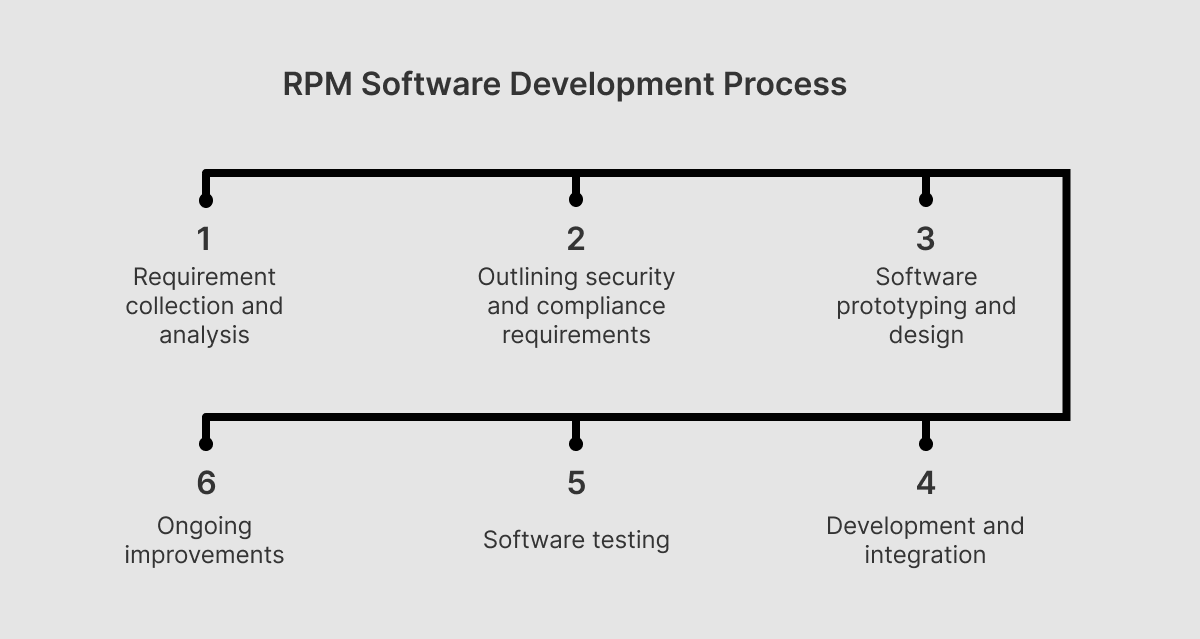
Step 1: Requirement collection and analysis
The development process starts with filling the gaps in your product vision and setting the context for further development. At the initial stage, your software development team collaborates with you to define project goals and requirements based on the specific health conditions your RPM will target.
Following the requirements, your development team helps you identify core functionalities, choose the optimal technology stack, and plan the application architecture. If your RPM solution integrates with other healthcare systems, such as EHRs, your technology partner will help you design integrations.
Step 2: Outlining security and compliance requirements
Remote patient monitoring software handles healthcare data in transit and at rest, which is subject to regulations such as HIPAA and FDA regulations, so designing for compliance and security requirements is necessary and will save you a lot of trouble down the road.
Based on your compliance needs, your development team incorporates audit trail capabilities into the development process and selects robust encryption protocols to protect sensitive data. At this stage, developers also choose secure and compliant cloud data storage and identify an API to enable uninterrupted communication between the backend, client applications, and IoT devices. Here, your team also pinpoints an optimal testing strategy for pre- and post-production releases.
Step 3: Prototyping and design
To create a user-first, intuitive interface, your UX/UI team conducts user research to shape user personas and their journeys. Building on the research, designers transform your initial vision, combined with user needs, into a tangible representation of the platform (prototype) to get stakeholder and user feedback on the look and feel of the future software product. When creating interface designs, your team should prioritize a clean interface that is both engaging and accessible to all users.
Drawing on the user feedback, your design team refines the prototype and finalizes the designs. Polished design layouts are provided to the development team for reference.
Step 4: Development and integration
Your RPM system is iteratively developed with a focus on regulatory compliance. The development scope may include frontend and backend development, mobile app creation for patient use, doctor-facing app development, and integration with medical devices.
Step 5: Testing
When it comes to RPM development, thorough software testing is as important as the development itself. Along with thorough testing activities, developers should prioritize IoMT device compatibility and smooth integration with the RPM system to achieve the best stability possible.
Step 6: Ongoing improvements
After deployment, your development team monitors the performance of your RPM system and fine-tunes it to align with your specific business and technology requirements. To facilitate adoption, your tech partner can assist in user training by providing comprehensive training materials and ongoing support for both patients and healthcare professionals.
Along with ongoing system monitoring and troubleshooting, your tech team prepares a roadmap for software updates to continuously enhance the system’s features and security.
Challenges in implementing RPM software and how to clear them
Virtual care has the potential to reduce costs, slash workloads, and push the boundaries of traditional care, but those benefits come with their own set of tech considerations. Unless addressed, these considerations can hinder the implementation of RPM solutions and introduce additional risks and hurdles, making your RPM system a liability rather than a competitive advantage.
Data security and privacy
RPM solutions collect sensitive patient information, which is then transmitted between devices, apps, and servers. This system itself increases the attack surface, as potential weaknesses in transmission, storage, and access to RPM data can compromise the security of PHI. RPM devices can also be susceptible to tampering if not adequately secured.
To address these threats, it's crucial to implement robust security measures, including:
- Encryption of RPM-collected data, telehealth appointment recordings, and other sensitive patient health data.
- Strong authentication and role-based access.
- Regular audits and security assessments.
- Employee and patient training.
- Audit trail.
Combined, these safeguards can offset data security risks and promote a secure IoMT environment. Keep in mind that while security is a crucial component, it’s important to keep RPM software easy to use, as overly complex systems can adversely affect user experience.
The issue of data privacy also remains a significant adoption hurdle, as patients’ trust in virtual care depends on robust data privacy measures. Addressing this issue requires healthcare teams to include informed consent for data collection, storage, usage, and sharing in the RPM systems. Patients should be put in control of their data, having a clear understanding of who has access to it. Data anonymization can also mitigate privacy risks and build trust with patients.
Reliability and connectivity
To transmit data in real time, RPM devices require a stable internet connection, which may not be available to patients in remote areas or with poor internet infrastructure. Battery depletion, software glitches, slow processing times, and hardware failures can also impact data transmission, leading to data loss, delays, and disruptions in monitoring.
To improve the system’s reliability, your RPM ecosystem should implement redundancy measures, such as multiple communication channels and an offline mode of operation with batch operations, where needed, that will help mitigate connectivity issues. The system should also employ low-power protocols to reduce energy consumption, while regular maintenance and software updates can help maximize device efficiency and foster smooth data transmission.
Performance efficiency
As the number of patients increases, the system needs to adjust to the growing data processing workloads. Additionally, some RPM systems require real-time data processing of critical health parameters. Cloud-based solutions can deliver the performance efficiency (scalability and flexibility, to be exact) your platform needs to provide just the right amount of resources for the demand at every point in time. Also, data compression and optimization techniques can optimize storage requirements and enhance the processing efficiency of your RPM solution.
Patient adoption and training
The long-term success of RPM programs depends on the engaged patient population and the level of patients’ health literacy. Approximately 36% of adult Americans have only basic or below-basic health literacy skills, leading to difficulties interpreting RPM device data and missed readings. That’s why your RPM system needs to be designed with clear instructions and user-friendly interfaces to cater to patients with varying levels of health literacy.
Patient-facing educational materials, training documentation, and motivational strategies, such as setting goals, providing feedback, and offering advice on healthy behavior changes, will help you win over patients and overcome adoption barriers.
Workflow integration and interoperability
Health system fragmentation — the one caused by disparate healthcare software platforms — can also impede the successful implementation of RPM. To facilitate timely access to data and prevent delays in clinical decision-making, virtual care systems must integrate seamlessly with existing workflows, which is challenging without data standardization. Differences in data formats hinder the import, analysis, and display of RPM data in other healthcare systems.
To achieve data compatibility, an RPM system should be developed in accordance with common health data formats such as FHIR, HL7 v2 and v3, ICD-10, and others, as well as implement standardized APIs specifically for RPM integration.
Regulatory compliance
Arguably, the most complex challenge facing any type of health technology, and RPM, in particular, concerns regulatory compliance. As RPM devices collect, transmit, and store protected health information, they are subject to global and local healthcare regulations, HIPAA, FDA, and GDPR being the most common among them. To avoid legal jeopardy, healthcare providers must ensure that their RPM systems meet stringent compliance requirements and implement robust data security and privacy mechanisms.
Software quality also has a strong influence on regulatory compliance, which makes rigorous quality assurance a must for the development of RPM software. For compliance purposes, your technology partner should also have comprehensive software documentation in place and strictly follow ISO 27001 and IEC 62304 requirements during development.
How much does it cost to develop RPM software?
There is no single formula for calculating the cost of developing patient monitoring software. It’s a combination of cost drivers, such as your project scope, complexity, regulatory requirements, and device integration, that impact your tech investment. The development approach (in-house or outsourcing) and the location of your development team also affect the pricing.
Below, you can see a table with ballpark estimates for an RPM platform put together by our experts based on our previous projects. The estimates are based on the average hourly rate of $50/hour.
| Features | Approximate time, hours | Approximate cost, $ |
|---|---|---|
Mobile (Patient-Focused) | ||
| Project setup | 111 | 5,566 |
| Authentication/Registration | 63 | 3,128 |
| Profile management | 61 | 3,030 |
| Manual data entry | 42 | 2,121 |
| List of clinicians | 18 | 909 |
| Cliicians profile | 15 | 758 |
| Device integration | 64 | 3,182 |
| Patient dashboard | 36 | 1,818 |
| Push notifications | 36 | 1,780 |
| Messaging | 73 | 3,636 |
| Compliance and security | 76 | 3,795 |
| Deployment and integration | 67 | 3,333 |
| Basic analytics | 45 | 2,235 |
Web (Clinician-Focused) | ||
| Project setup | 61 | 3,036 |
| Authentication/Registration | 57 | 2,825 |
| Profile management | 31 | 1,568 |
| Clinician dashboard | 97 | 4,848 |
| List of patients | 18 | 909 |
| Patient profile management | 61 | 3,030 |
| Notifications | 18 | 909 |
| Messaging | 27 | 1,364 |
| Reports | 109 | 5,454 |
| Compliance and security | 63 | 3,163 |
| Deployment and integration | 121 | 6,060 |
General | ||
| Admin panel | 100 | 5,000 |
| Design | 170 | 8,500 |
| Product discovery | 120 | 6,000 |
| Total | 1,759 | 87,950 |
Keep in mind that our estimate focuses solely on the development costs of a minimum viable product. By building an MVP first, you can validate your product concept early and gather valuable user feedback needed for full-fledged development.
Embracing a new era of patient well-being with RPM software from Orangesoft
As a healthcare software development partner with 15 years of experience, our company is keenly aware of the unique context of the healthcare industry. We possess extensive experience developing healthcare software solutions, including virtual hospital platforms, medical device apps, telemedicine solutions, and more.
At the core of every healthcare software project we implement lies our unwavering commitment to the following requirements:
- Data security and regulatory compliance with HIPAA, HITECH, PIPEDA, GDPR, FDA, and ISO standards.
- Thorough quality assurance of each deliverable to maximize the software quality, performance, and reliability.
- A dependable, scalable software architecture that seamlessly integrates into the existing healthcare tech ecosystem.
- Adherence to ISO 27001 and IEC 62304 requirements.
- Adherence to well-architected best practices to maximize software operational excellence, reliability, performance efficiency, cost optimization, and security.
- Seamless integration with various EHR/EMR systems.
By collaborating with us, you gain a trusted tech partner with proven expertise in healthcare projects, a development team trained in healthcare industry specifics such as regulations, use cases, and trends, and a full suite of development services to transform your vision into reality.
