By 2030, the Centers for Medicare and Medicaid Services (CMS) expects all Traditional Medicare beneficiaries and most Medicaid beneficiaries to be in accountable care relationships. But the transition to value-based care arrangements turned out to be quite a challenge for healthcare professionals who had grown into the traditional fee-for-service model. To that end, remote patient monitoring (RPM) solutions are stepping in as the critical link connecting patients to value-based care delivery.
Delivering longitudinal health data on vitals, adherence, and lifestyle metrics, RPM platforms enable doctors to monitor patients between visits, reduce ER visits, and improve patient outcomes — all pillars of the value-based care model.
Key takeaways
- RPM devices are the centerpiece of remote patient monitoring programs whose true value is unlocked when they are paired with companion web platforms, mobile apps, and clinician dashboards.
- The selection of RPM devices depends on the conditions being monitored, while their connectivity configuration — Wi-Fi, Bluetooth, or cellular — boils down to the tech specifics of the program and patient access to the network.
- A bidirectional connection between RPM and EHRs is crucial, yet that seamless link can be challenging to establish because of differences in data formats, misaligned workflows, and outdated EHR architectures.
What is remote patient monitoring (RPM)?
Essentially, remote patient monitoring is a type of telehealth that allows healthcare providers to monitor the physiological conditions of patients outside healthcare settings through at-home and mobile devices. Based on the devices in the mix, RPM systems can collect various types of data, including oxygen level, high blood pressure, or any other physiological metrics.
Traditionally, remote patient monitoring was used to keep an eye on patients with acute and chronic conditions, from diabetes patients to those with hypertension and heart failure.
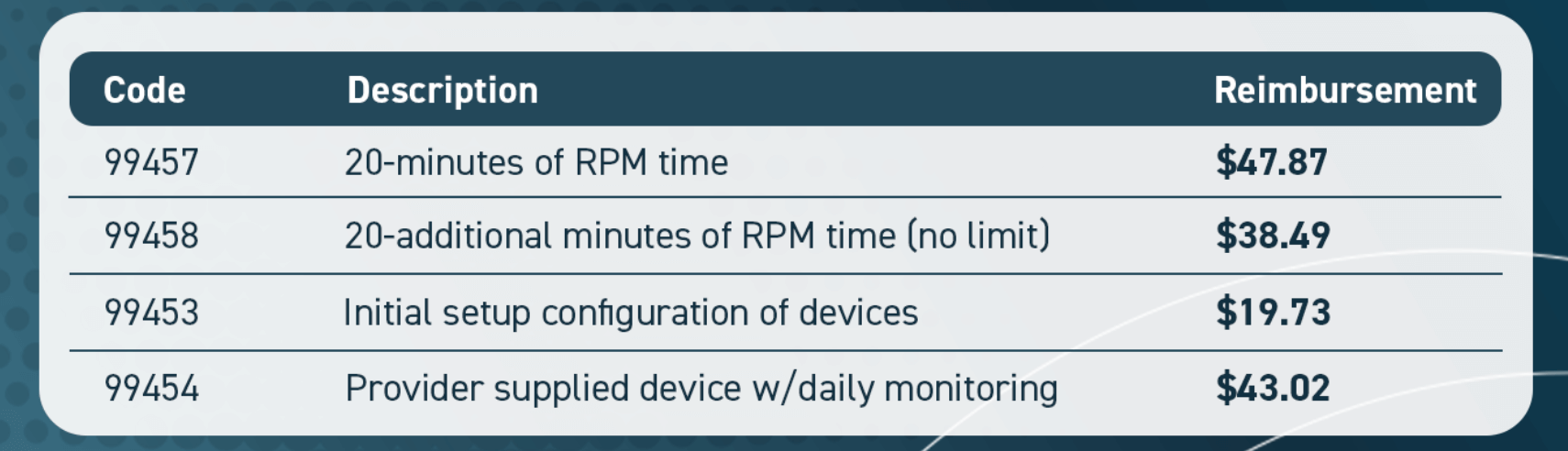
Today, RPM solutions are being integrated into the value-based patient care model and applied across various specialties, including preventive care, post-surgical recovery, medication adherence, and even lifestyle interventions. CMS already has RPM CPT codes, such as 99453, 99454, 99457, that reimburse providers for remote monitoring.
How RPM works: from device to dashboard
RPM runs as a multi-step workflow that relies on the interplay of several technologies to collect patient data, transmit it securely to healthcare providers, and inform proactive interventions based on the analyzed data.
Initially, all patients get onboarded onto the RPM platform, with devices paired to make sure the data flows into the system with no interruptions. The step-by-step process of RPM includes the following steps:
- Data collection at the source — Connected devices capture vital signs or health metrics.
- Data transmission — The data is sent over to a paired RPM app or RPM hub via Bluetooth, Wi-Fi, or cellular networks.
- Data aggregation — RPM platforms collect inputs from multiple devices and standardize them into usable formats. Encrypted data is then sent to cloud-based systems or pushed directly into electronic health records for storage and access by healthcare providers.
- Data analysis — Smart algorithms can then comb through the insights and bring health trends, anomalies, or threshold breaches to the clinician’s attention.
- Clinical intervention — Care teams review the flagged insights and perform the necessary intervention, whether that’s dose adjustments, escalations, or follow-ups.
- Patient engagement — Patients can use paired mobile applications to get tailored feedback, reminders, or educational prompts, based on the collected data and clinical input.
If that’s an AI-powered RPM platform, it continuously learns from the data to improve monitoring thresholds and elevate recommendations.
Why RPM devices matter in modern healthcare
RPM offers a clear return on investment over time, but the ROI of remote monitoring is not reimbursement — it’s the outcomes.
Benefits for providers
For healthcare providers, the effectiveness of RPM programs depends on the condition and provider engagement with the data, along with their ability to act on that data. Overall, remote patient monitoring is a win for healthcare providers because:
- RPM tools reduce ER visits and hospital readmissions — Studies show that large-scale remote patient monitoring programs can reduce hospital admissions by 59% across multiple diagnoses, including congestive heart failure and hypertension.
- Remote patient monitoring improves patient outcomes — According to a study, uncontrolled hypertension dropped from 66.3% to 40.2% after 90 days on the RPM program.
- RPM systems enable data-driven clinical decisions — Thanks to continuous streams of patient health data, providers can tailor their patients' plan of care and proactively intervene to avoid complications.
Benefits for patients
The benefits of remote patient monitoring are not limited to the provider side of care. Over 80% of patients reported a high willingness to use remote patient monitoring, which is unsurprising considering the tangible benefits such programs can deliver:
- Convenience — With RPMs, patients don’t have to make clinic visits, since they can take measurements from the comfort of their own homes.
- Easier adherence — Many RPM platforms include patient engagement features such as educational content, personalized feedback, and reminders to actively engage patients and improve treatment plan adherence.
- Proactive health management — Connected RPM apps usually send real-time feedback on vital signs and lifestyle metrics, enabling patients to take active control of their health management and make informed choices about lifestyle, diet, and activity.
Ten tools that drive remote patient monitoring
Through RPM, care teams can oversee multiple acute and chronic conditions, and the selection of RPM tools can vary accordingly. Here are ten of the most common and impactful devices that can be integrated into RPM projects.
Blood pressure monitors

Typically used for hypertension management and cardiovascular monitoring, modern blood pressure monitors are digital cuffs that send blood pressure readings straight to a paired RPM platform. Blood pressure data usually flows directly into the patient’s electronic health record.
Unlike in-office measurements, blood pressure monitors take measurements daily, helping providers spot masked hypertension or early signs of cardiovascular risk. Clinicians can also set a minimum BP threshold for each patient. If the patient’s blood pressure is not within the set range, the system automatically flags the reading for review.
Blood glucose meters (BGMs) and continuous glucose monitors (CGMs)

Blood glucose meters and CGMs are devices designed for managing diabetes and other metabolic conditions. The two devices take different approaches to measurements. Blood glucose meters measure point-in-time glucose levels in blood using a small drop of blood. CGMs measure blood sugar continuously in the fluid underneath the patient’s skin through a small sensor placed there.
Because of this difference, blood glucose meters are usually used for patients with less intense regimens, while CGMs support condition monitoring in higher-risk contexts, such as type 1 diabetes. By the same token, many RPM programs start with BGMs for larger patient groups, because they are less costly and easier to integrate. Conversely, CGMs are used selectively for high-risk patients.
Pulse oximeters

Cellular-connected pulse oximeters capture blood oxygen saturation levels and heart rate, with the readings usually synced in near real-time with apps, clinical portals, and EHRs. Typically used for chronic respiratory conditions like chronic obstructive pulmonary disease, asthma, and pneumonia, pulse oximeters help doctors identify and escalate deteriorating patients to avoid invasive ventilation and unnecessary ICU readmission.
Like other RPM devices, pulse oximeters deliver longitudinal SpO2, which, compared to spot checks, is a better fit for proactive care. In advanced RPM platforms, pulse oximetry data can be combined with blood pressure and weight data to identify worsening conditions.
Digital thermometers
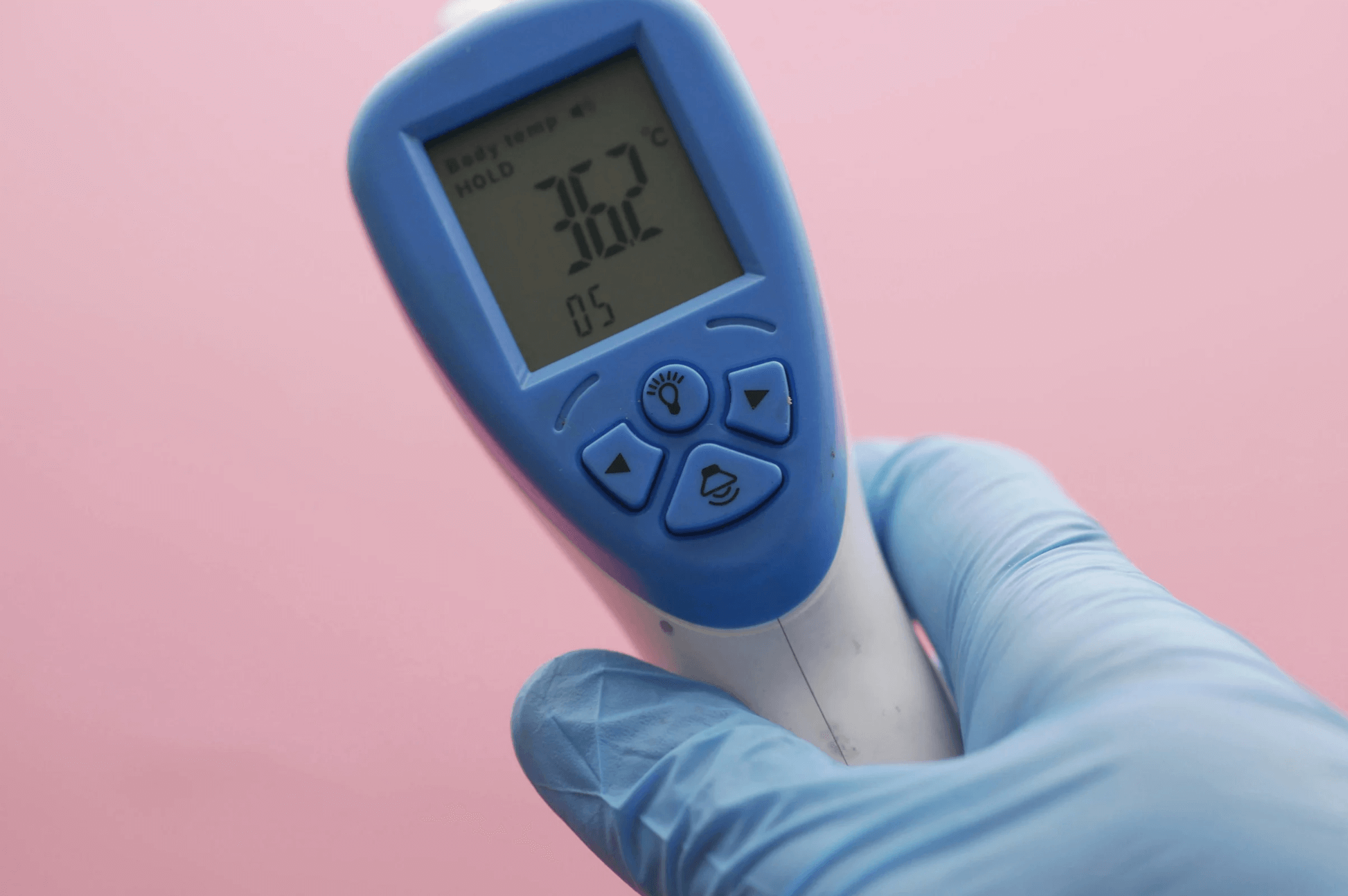
Fever is a common indicator of illness, worsening symptoms, or infection, which makes continuous body temperature monitoring a viable component for RPM programs. Typically connected to cellular networks, modern digital thermometers use a 1-second measurement to track body temperature.
Although thermometers might come across as a basic household device, RPM takes the utility of these devices to the next level. Instead of patients jotting down readings, body temperature data flows automatically into the platform for trend analysis. Paired with other vitals, temperature data adds context for clinicians to catch complications early.
Digital weight scales

Weight might seem like a simple number, but in remote patient monitoring, it tells a much bigger story. For patients with heart failure, kidney disease, or obesity, daily weight fluctuations are an important indicator that can hint at fluid buildup and potential complications. That’s why digital weight scales have become frontline devices in remote patient monitoring.
Connected digital scales transmit each measurement to the RPM platform. Supplemented with other vitals like blood pressure and SpO2, weight data allows for a more nuanced clinical analysis of an individual’s cardiovascular health. For patients, seeing their weight trends on a paired app can be a strong stimulus for keeping up with the healthy lifestyle and prescribed activities.
ECG/EKG monitors
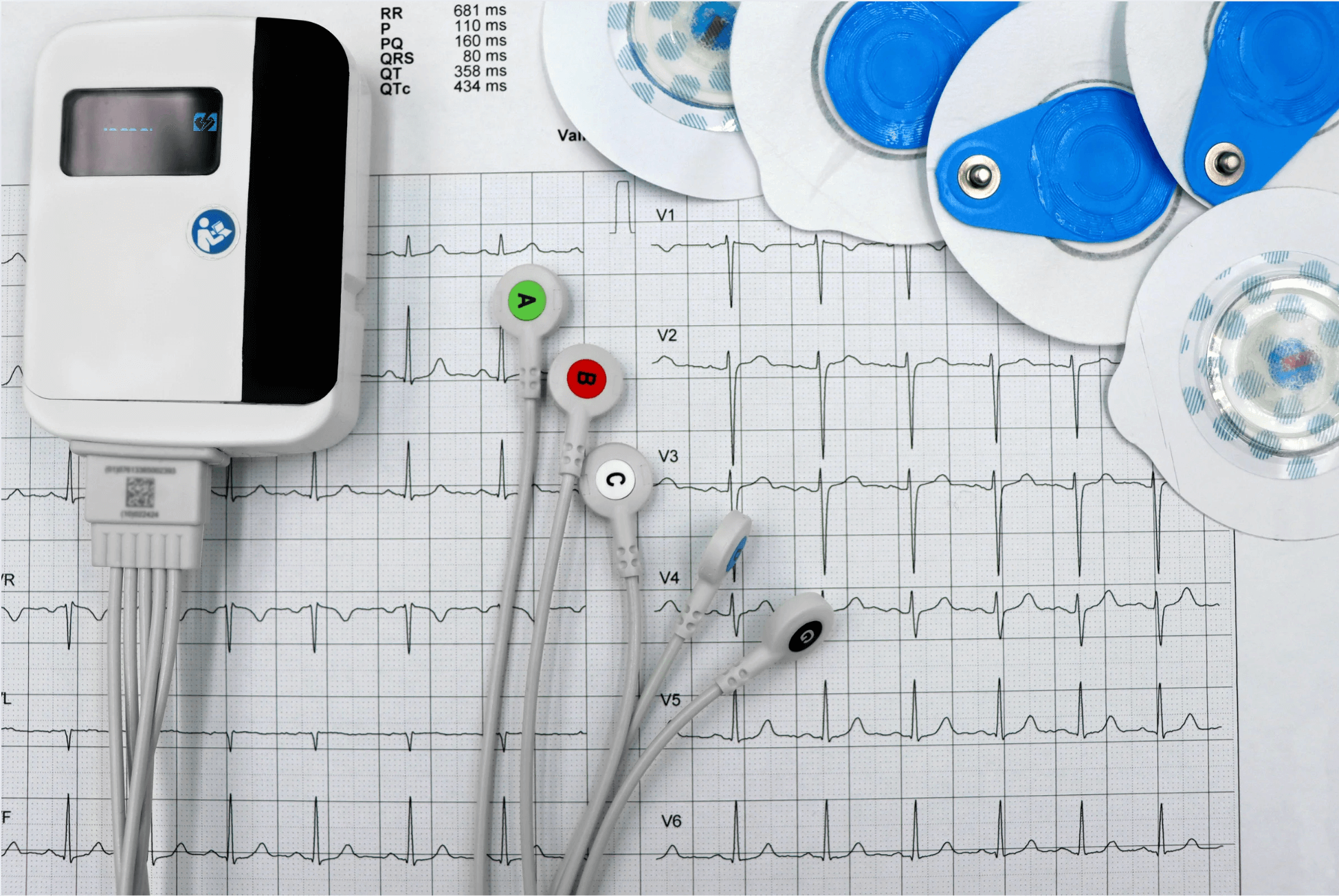
ECG/EKG monitors record electrical activity of the heart, which makes them a crucial companion device for individuals with arrhythmias, atrial fibrillation, or other rhythm disorders. In RPM settings, ECG/EKG monitors can be either wearable or handheld. Regardless of their form, they are used with a unified goal of capturing heart rhythms over time and sharing that data with the synced RPM platform and apps.
Since this type of data is dense, integration and visualization play a strategic role here. Care teams need easy and quick access to clinically relevant insights, which can be ensured with AI filters and clinician-defined alerts. Integrating with the EHR is another rule of thumb here to make sure clinicians can pull up that data right within their existing system of use.
Spirometers

Spirometers determine how well the patient’s lungs work by measuring the amount of air the patient inhales and exhales. Traditionally refined for pulmonary clinics, spirometers have become the mainstay in remote patient monitoring because of their ability to track metrics like FEV1 and FVC within home settings. Captured over time, this data allows care teams to forecast Chronic Obstructive Pulmonary Disease exacerbations and adjust treatment before it’s too late.
Home-based incentive spirometry also steps in for post-operative and post-transplant monitoring, asthma management, and diagnostic support. The effectiveness and data accuracy of spirometers in RPM depend on how well the patient can perform the maneuver. For this reason, many spirometers are marketed with companion apps that educate and guide patients through each procedure.
Wearable activity trackers

Digital health trackers, the gadgets usually associated with basic step tracking, can also add valuable new dimensions to remote tracking. Fitbit, Apple Watch, and other wearable trackers can help patients log basic human vitals, such as sleep patterns and physical activity, as well as advanced physiological parameters like heart rate variability, oxygen saturation, and stress levels.
In RPM programs, activity trackers are indispensable for monitoring patients with chronic diseases and, more importantly, for understanding which lifestyle factors have the greatest impact on health outcomes. Stacked alongside other vitals, data from wearables adds more context to health events. For example, a spike in blood pressure is more clinically meaningful if it happens simultaneously with an elevated heart rate.
Medication adherence monitors

When it comes to patient adherence to prescribed regimens, it’s a decision patients get to make most of the time. If patients fail to stick with the regimen, this can render even the most tailored care plans ineffective and lead to needless, potentially harmful treatment escalations. Smart dispensers, connected pill bottles, ingestible sensors, and other devices help ensure that patients take their medication consistently and as prescribed.
In RPM, such devices provide objective data about medication-taking behavior through timestamped records rather than relying on self-reported adherence information. More advanced monitors can even notify healthcare providers when patients are non-compliant.
Remote fetal monitoring devices

With uterine activity monitors and fetal heart rate trackers, physicians can conduct fetal non-stress tests for expectant mothers remotely. The maternal-fetal health data from such devices streams directly to the RPM platform and the EHR, allowing obstetrics providers to monitor high-risk pregnancies and post-operative patients from afar and within a single interface.
Compared with intermittent monitoring, continuous fetal health tracking enables early detection of abnormal parameters and potential complications, giving obstetricians more lead time to intervene than the standard two-week appointment schedule allows.
Connectivity and integration considerations for RPM devices
Remote monitoring is only as effective as the reliability of systems behind it. To deliver value, RPM devices have to be securely integrated into the actual fabric of care, stay consistently connected, and constantly push data in the background. Without all this, even the most sophisticated devices can become a burden rather than a benefit.
How RPM devices connect: Bluetooth, Wi-Fi, cellular
RPM devices can leverage different types of connectivity, depending on the device specs, the clinical environment, and the patient. Each connectivity approach has its pros and cons:
- Bluetooth
Bluetooth-enabled communication is widely used for short-range connections between a device and a patient’s smartphone or an RPM hub. Such RPM devices as glucose monitors, blood pressure cuffs, and thermometers often rely on this type of connectivity because it’s low-power and smartphone-friendly.
However, Bluetooth-based connections may be prone to the last-mile data problem: if the patient’s smartphone is off or out of range, the data flow is interrupted. Also, this type of connectivity is sensitive to interference from other electronic devices. That’s why a short-range Bluetooth connection is more suitable for intermittent monitoring, where proximity to the device is not an issue.
- Wi-Fi
Wi-Fi uses radio waves to connect RPM devices to a local network, which then sends the data to cloud platforms and healthcare providers over the internet. This connectivity configuration enables high-speed data transfers, allowing for near real-time insight sharing for RPM devices that transmit large volumes of data or require frequent updates. ECG monitors, smart scales, and sleep trackers
However, the connection reliability is hard to predict as bandwidth limits, network interruptions, and weak signals can all affect the data transmission capability. To that end, many Wi-Fi-enabled RPM devices are equipped with built-in safeguards, such as local data buffering and automatic reconnections, among others, to compensate for the inherent downside.
- Cellular
Similar to mobile phones, cellular RPM devices rely on mobile networks, like 3G, 4G, and 5G, to hand the data over. Out of the three, this type of connectivity is considered to be the most reliable, as it doesn’t require smartphones or an internet connection. It’s the gold standard for high-risk patient populations, older individuals, and those living in rural or remote areas. However, this type of connectivity can be costly since it often requires a dedicated data plan for each device.
Interoperability and integration with EHRs and care platforms
Unless the data flow directly into the EHR and other related platforms, it’ll remain locked behind the RPM system, out of sight and out of reach for clinicians. Precisely for this reason, the RPM system and the EHR must be interoperable and use standardized communication protocols. It’s a prerequisite that is often challenging to achieve, because of:
- Different data formats — the data formats between an EHR and an RPM aren’t always compatible by default, which makes it hard for an EHR to decipher vitals from devices. To sync RPM device readings into the clinical records, integration developers need standardized protocols such as HL7 FHIR. In most cases, developers build middleware to translate device data into an EHR-readable format. Test readings before deployment also help validate that timestamps, units, and patient identifiers are recorded correctly in the EHR.
- Legacy systems — Older EHRs aren’t cut out for RPM programs, since they don’t have modern APIs and integration capabilities baked in. Developers usually layer in middleware integration engines to make up for the lack of built-in connection and get the data flowing.
- Workflow mismatches — Clinicians already have way too many screens on their hands, so another couple of extra clicks or a standalone RPM dashboard can become another bottleneck. Integrating RPM data into the existing workflow makes RPM data easy to see and act on for care teams.
Must-have security and compliance measures for RPM setups
Remote patient monitoring devices collect significant volumes of sensitive patient information to oversee the patient’s health status. In this high-stakes scenario, keeping that data under lock and key is non-negotiable. As healthcare software developers, here are the crucial safety nets we implement in RPM projects to keep the data secure and give peace of mind to doctors and patients:
- HIPAA/GDPR compliance — The RPM system must be implemented in accordance with local and regional healthcare compliance requirements, such as HIPAA for US-based settings, and GDPR for systems operating in the EU.
- End-to-end encryption — All data sent from RPM devices to cloud platforms and EHRs must be encrypted in transit and at rest.
- Device-level authentication and secure APIs — Only authorized devices can connect to the system, with each RPM device being granted a unique digital identity or certificate that the system verifies before accepting data.
- Access control — Role-based access control, multi-factor authentication, and the least privilege principle keep the RPM system shielded from unauthorized users.
- Audit trails — Thanks to this security measure, care teams can achieve full accountability in terms of who, when, and why accessed the RPM data.
This is not an exhaustive list of security measures. Data minimization, automatic patching, data backups, and other security measures create a multi-tier approach that not only keeps the patient data secure but also builds trust among both clinicians and patients.
Software that brings RPM devices to life
At their core, RPM devices are sensors that transmit raw numbers. They need companion software to contextualize those numbers in ways that support clinical decision-making. Here’s what the software layer might look like in RPM setups:
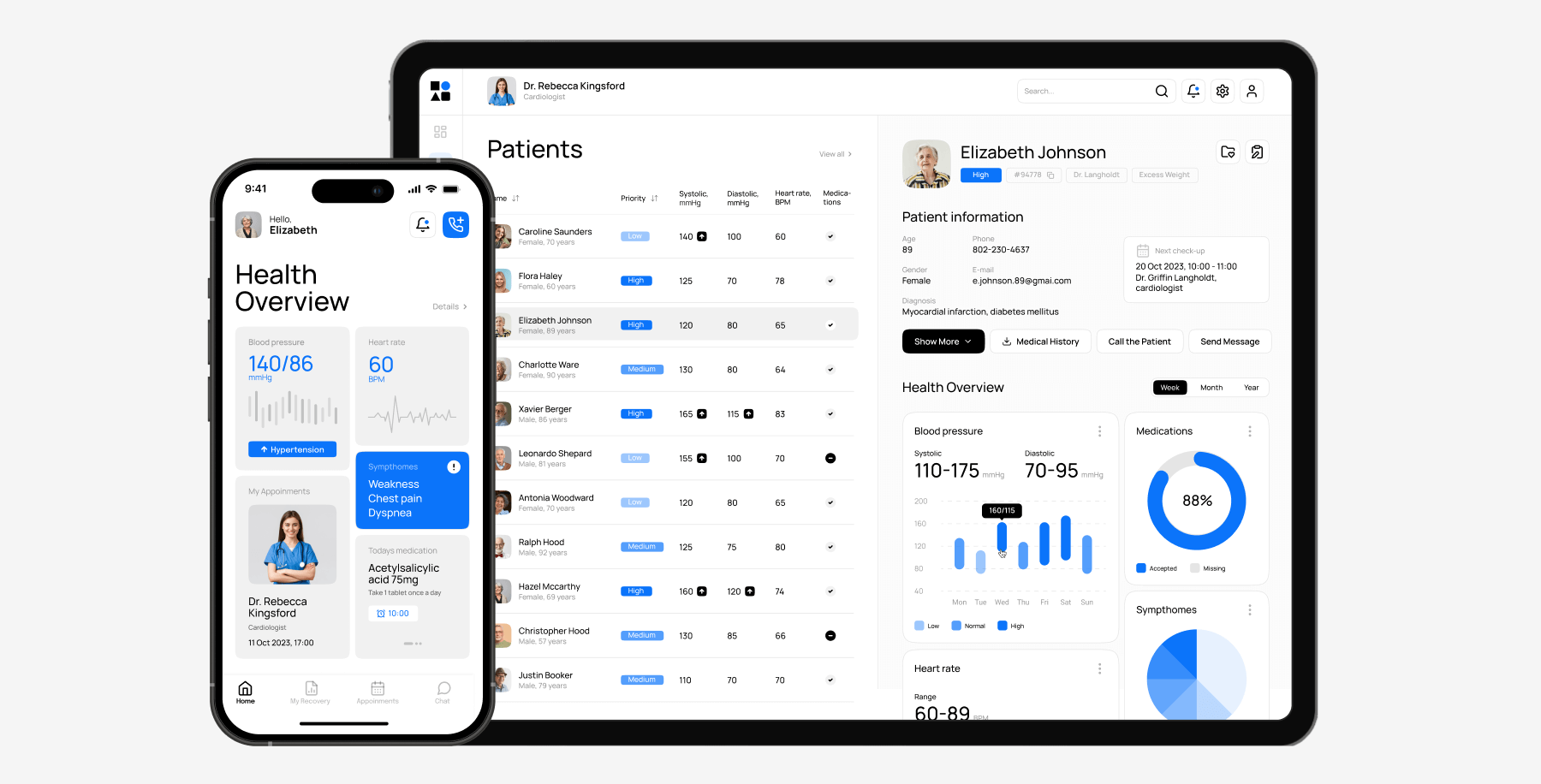
Mobile and web apps for patients and providers
Mobile and web interfaces act as a bridge between patients, RPM devices, and care teams. For patients, an RPM app can serve as an educational resource, a provider communication tool, and a daily health hub, where they can log symptoms, view trends, and stay on track with their medication thanks to reminders.
For providers, web- and mobile-based applications provide on-the-go access to key health metrics of patients and RPM workflows.
Alert systems and real-time dashboards
RPM devices generate a gigantic amount of data each day. With so much data pouring in, care teams need a way to cut through the noise and focus their efforts on high-priority action items. Alert systems and real-time dashboards do exactly that — they highlight what’s important and turn the daily data flood into something more digestible for healthcare professionals.
Any abnormality, whether that’s a blood sugar spike or unusual activity levels, will create an alert to prompt the care team to intervene. On the other hand, dashboards consolidate all RPM data and neatly organize it into a high-level view, with critical metrics highlighted. Care teams should have the ability to customize the dashboard layout and configure alerts for specific thresholds.
AI-driven insights and predictive analytics
The smart component of RPM, an AI engine within the RPM system, does the heavy lifting of continuous real-time analysis of patient metrics. AI algorithms can also spot warning signs early, predict health events, and tailor the interventions to the unique health profile. This layer of intelligence is a must-have for data-intensive RPM programs because it makes all interventions, actions, and care plans meaningful and proactive.
Orangesoft’s experience developing custom RPM platforms
Our company has been developing custom healthcare software since 2011. As a healthcare tech partner, we help innovative startups and established healthcare organizations take healthcare to the next level through the right combination of technologies.
RPM software is a core part of our portfolio. For one of our clients, we delivered an FDA-compliant platform designed to support a post-stroke patient monitoring program established by a renowned US hospital network. The solution consists of a dedicated web platform for medical staff and a connected mobile app for patients.
Our team made sure to implement end-to-end encryption, RBAC, two-factor authentication, and other security measures to make sure the solution is up to industry standards. We also helped the client with the necessary documentation for the FDA submission process and developed the solution according to HIPAA requirements.
Today, this RPM system supports the company in delivering effective post-stroke rehabilitation to over 50,000 patients across the US.
Conclusion
As health care progresses from a fee-for-service approach to a value-based model that’s focused on improving patient outcomes and reducing costs, remote patient monitoring facilitates that transition. Powered by RPM devices and supportive software, RPM systems pave the way for a continuous, proactive model that merges in-clinic care with online care delivery modes.
But the virtual care model still has miles to go. Outdated EHR systems, different data formats, resistance to innovation, and other hurdles keep RPM from scaling effectively. If you, too, are struggling to integrate RPM into the broader healthcare tech estate, Orangesoft can help. With our team as your partner, you can build interoperable and secure virtual care solutions that comply with applicable healthcare standards and deliver the value-based care patients deserve. Contact us today.
