Telemedicine apps have become essential tools in modern healthcare, transforming how patients access care and how providers deliver it. In 2024, over 116 million users turned to online doctor consultations worldwide, up from around 57 million in 2019. But as telemedicine grows in popularity, competition among telehealth providers intensifies.
It’s no longer about video conferencing and basic chat functionality. Healthcare providers and patients now expect telemedicine apps to deliver secure, seamless, and comprehensive experiences on par with face-to-face visits.
Drawing on over 15 years of experience in healthcare software development, our team has singled out essential features telemedicine software providers can’t afford to miss in their MVPs, along with advanced “tech moats” that help telemedicine apps stand out in a saturated market.
Key takeaways
- Must-have features for a telemedicine app are the building blocks that enable a usable, compliant, and user-centered experience for both patients and providers.
- Advanced telemedicine app features, such as AI triage, smart assistants, and digital therapeutic tools, are usually added in later product versions and require careful prioritization.
- The line between must-have features and extras is blurring these days, as the competition grows in the telemedicine space.
12 must-have features in a telemedicine app
Let’s say you’re just venturing into the field and looking to develop a basic but fully functional and compliant telemedicine app to test the waters. Here is a list of twelve core features to include in your MVP to cover compliance basics and essential clinical workflows:
Secure user authentication
Let’s start with a fundamental HIPAA requirement: secure user authentication. This feature keeps unauthorized users at bay, allowing only permitted individuals to access sensitive health data and app functionality.
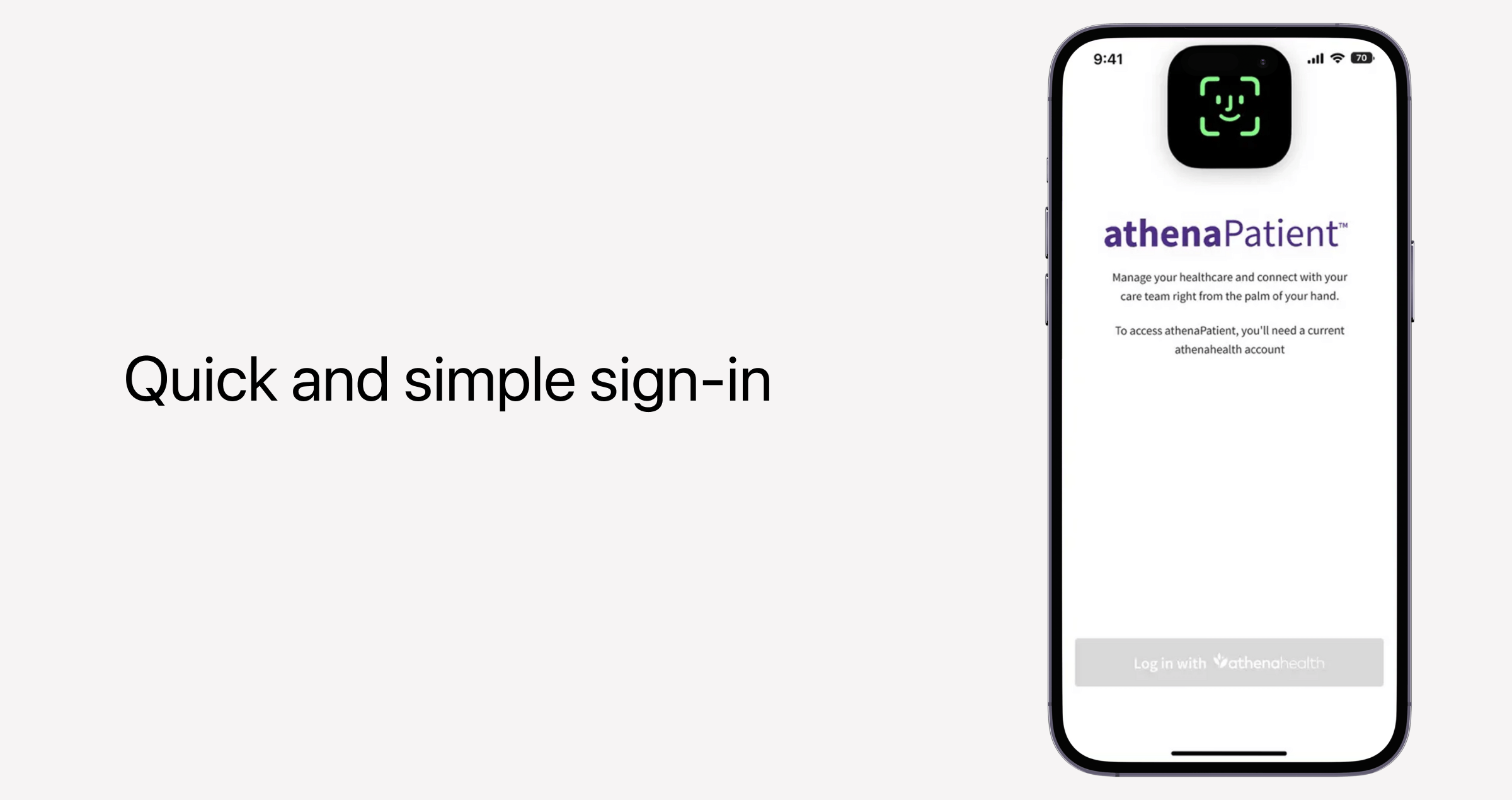
Techwise, user authentication is a combination of multiple safeguards:
- User registration and login — Users need to sign up to the platform using verified email addresses or phone numbers. All accounts are password-protected.
- Multi-factor authentication — Instead of just using their passwords to log into the systems, users must prove their identity with another verification factor, like an SMS code, email OTP, or authenticator apps.
- Role-based access control — Patients, providers, and admins only access features and data necessary to do their jobs.
- Encryption — Login details and sensitive information are protected with encryption at rest and in transit.
- Audit trails and monitoring — The system remembers logins, unsuccessful authentications, and unusual activity to spot potential threats and maintain a documented log for compliance audits.
Later, you can supplement this functionality with more sophisticated features like biometric login and single sign-on for providers.
Patient dashboard
Patient dashboards are a data-driven center of gravity for patients, with quick and easy access to relevant health information.
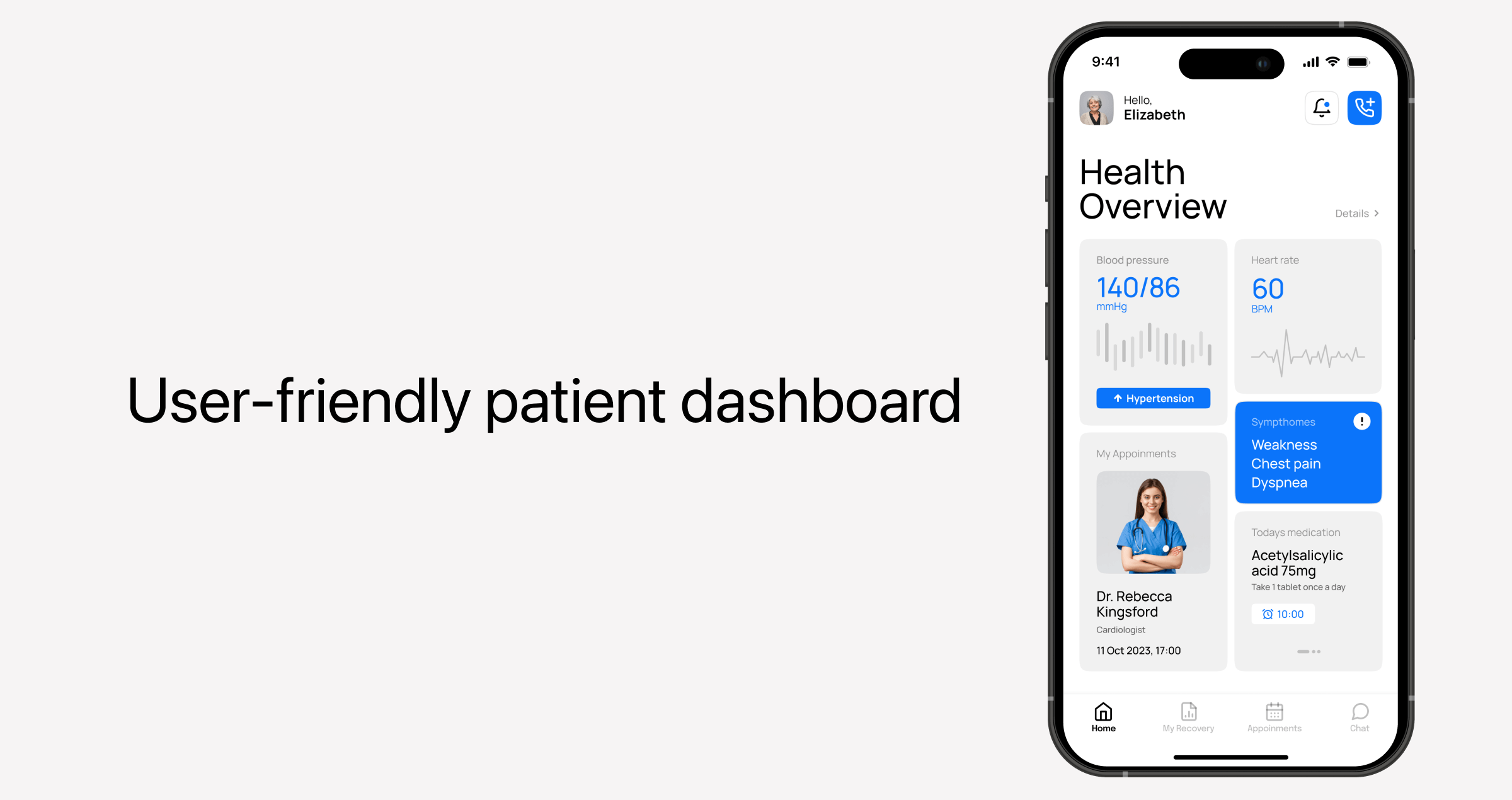
Dashboards vary in structure and design, but the majority include such data as:
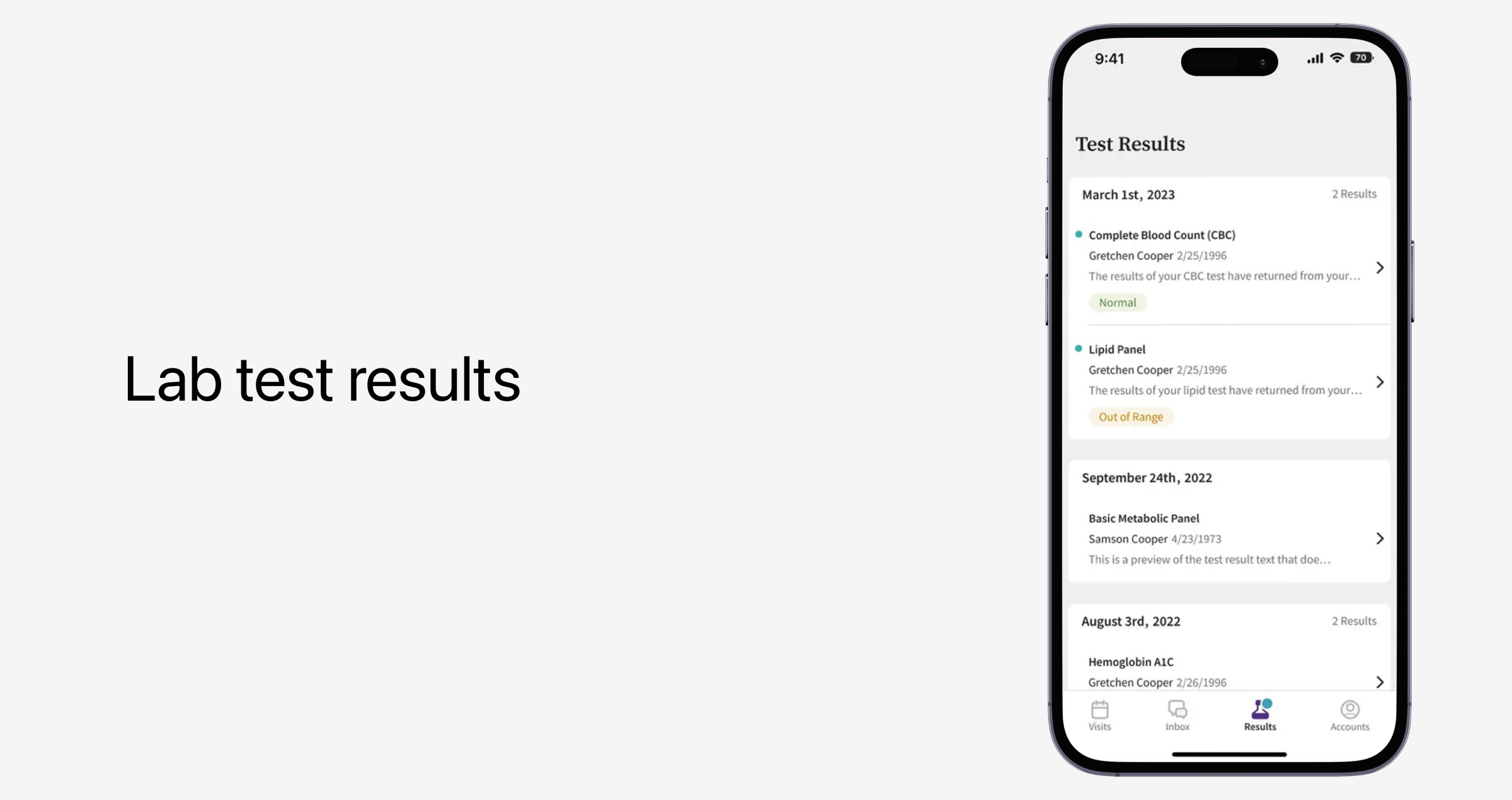
- Medical history — Patients can see the history of their past visits, diagnoses, test results, and prescribed treatments.
- Insurance information — Coverage details, co-pays, and billing information are also features on the dashboard. From a tech standpoint, this calls for integrations with third-party insurance APIs and measures to handle asynchronous data updates.
- Personal preferences — If a patient wants to customize notifications and app settings, they can do that in the dashboard.
Since dashboards integrate with various data sources, developers must ensure standardized data formats and enable real-time data streams without overloading the backend.
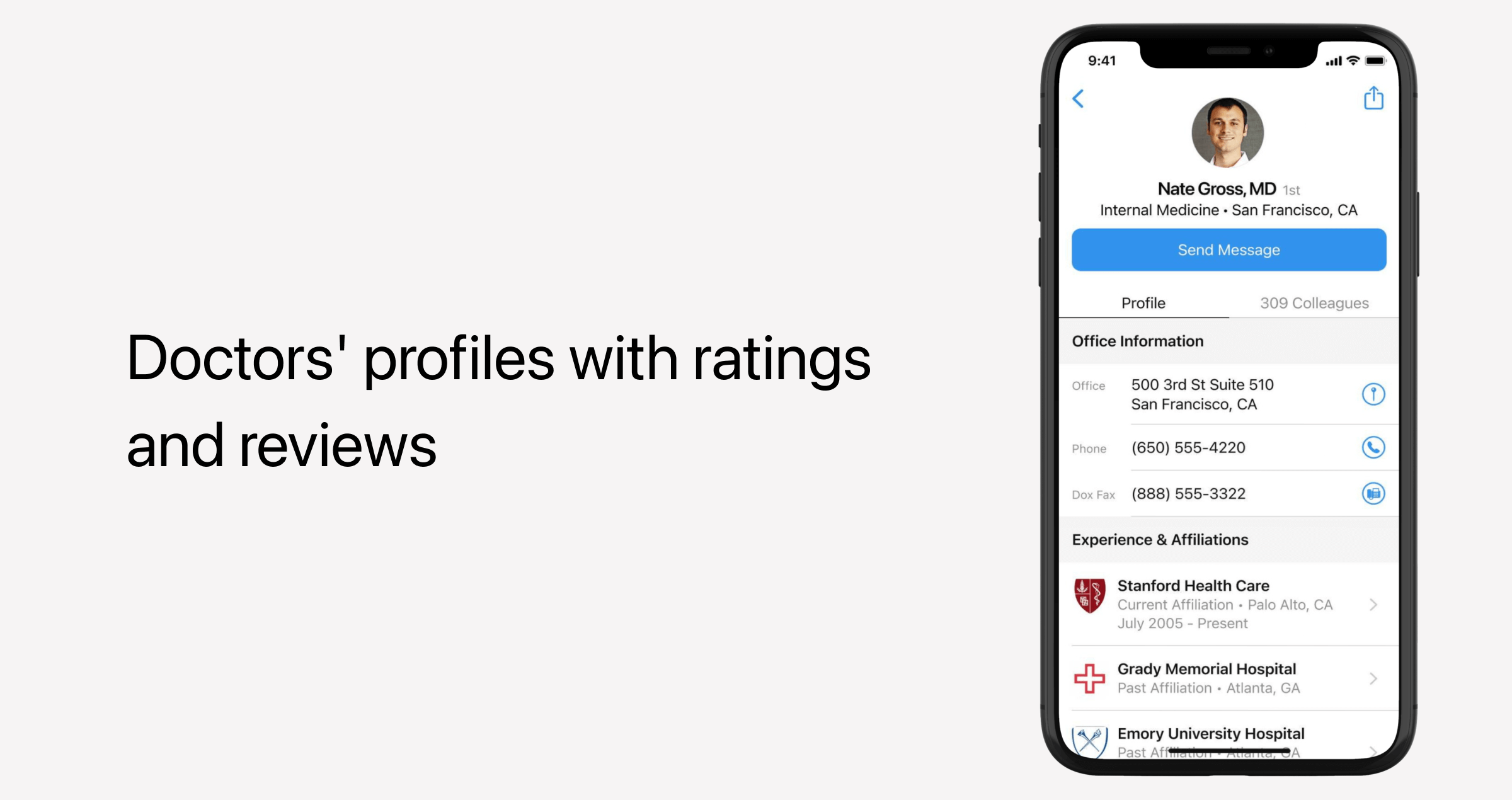
Services and doctors catalog
Most telemedicine apps include a searchable directory of medical professionals, where patients can see the services, free time slots, and types of appointments providers are open to. Having all options listed and filtered in one menu saves patients lots of effort and helps them locate the right provider quickly.
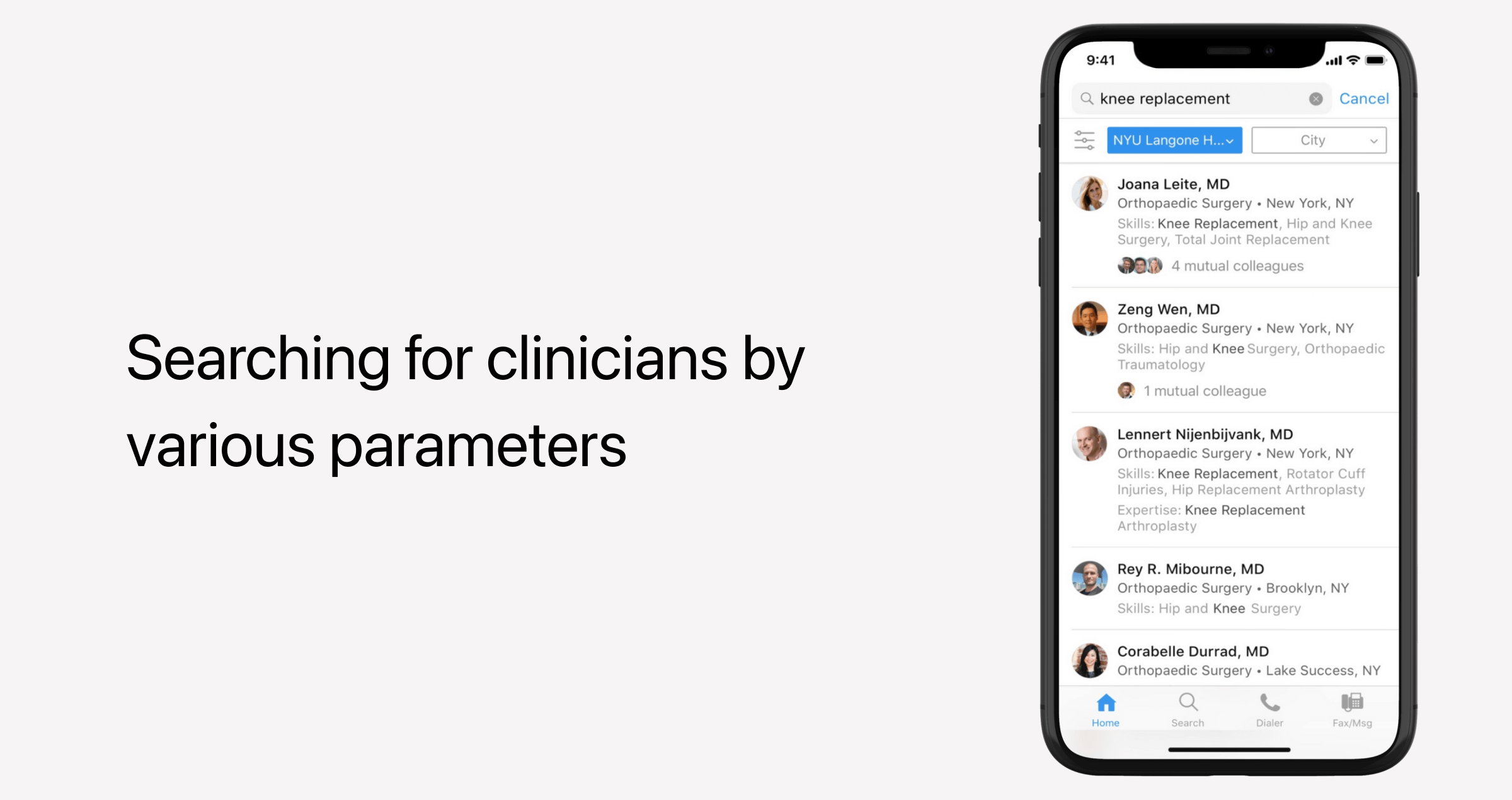
Make sure the catalog supports the following functionality:
- Service listings — The app makes it clear what types of medical care healthcare providers offer, whether that’s mental health or chronic disease management.
- Provider profiles — Patients can get to know their providers better before scheduling an appointment by viewing the credentials, specialties, experience, and ratings.
- Search and filtering — Patients can narrow down their options by specialty, availability, language, or insurance compatibility.
- Booking — Patients can book consultations, add themselves to waitlists, or set up recurring visits right from the catalog.
Provider dashboard and clinical tools
Both patients and providers need a unified data hub that keeps daily workflows, upcoming appointments, patient data, and clinical tools conveniently organized in one place.
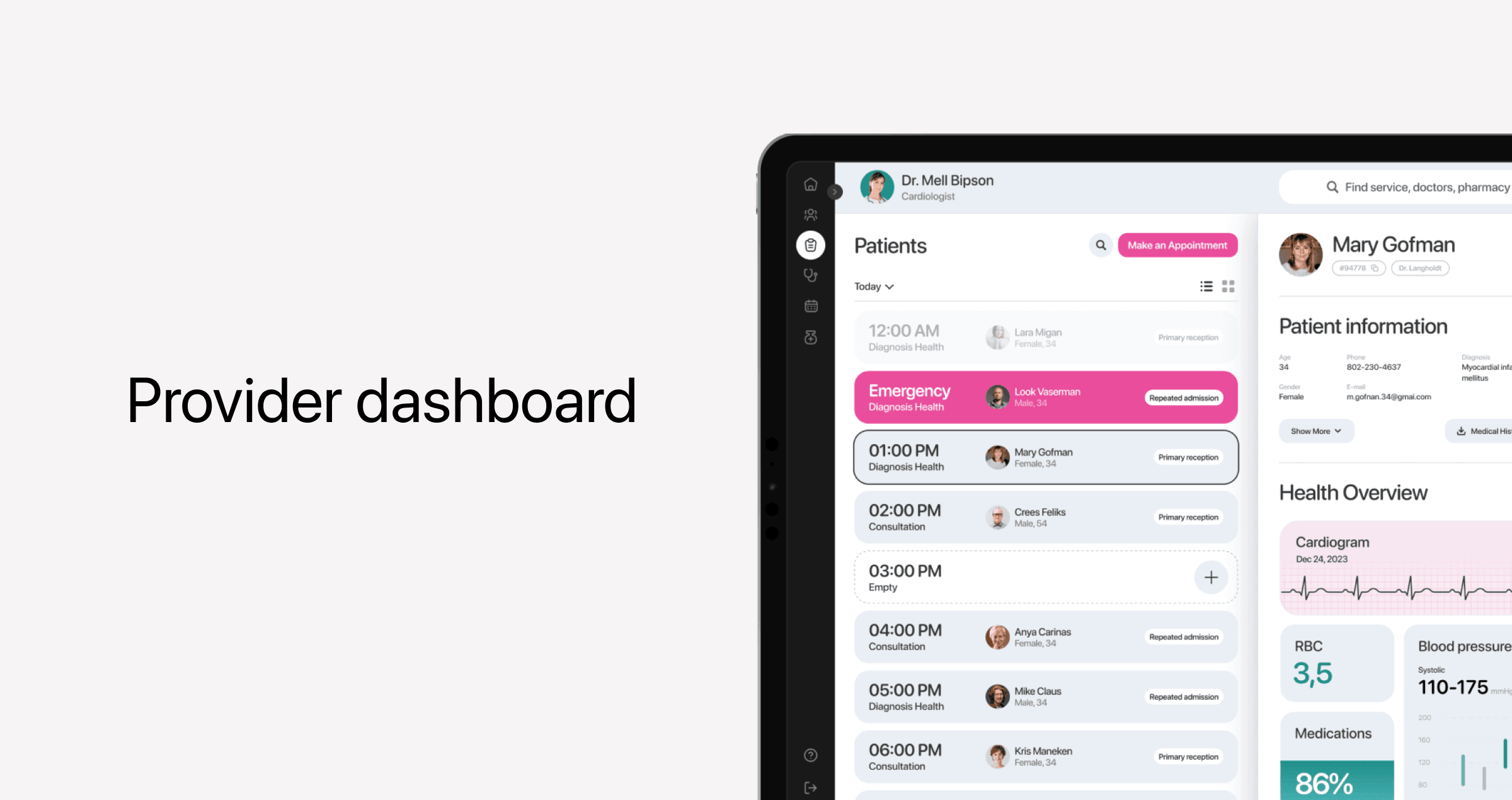
Provider dashboards usually consist of the following three components:
- Patient overview — Doctors need a high-level view of the patient's medical history, including diagnoses, treatment plans, allergies, and recent test results.
- Appointments — Dashboards typically include a section with upcoming appointments, including previews of key patient information, visit type, and status.
- Clinical tools — Providers should be able to create, edit, and store visit notes, e-prescriptions, and lab order referrals.
- Communication and coordination — The dashboard also offers a direct channel for patient-provider communication. Some applications also allow providers to connect with colleagues without leaving the system.
EHR/EMR integration
Early-stage telemedicine products can put this functionality on the back burner. But for provider-facing applications, a seamless data exchange with electronic health records is a non-negotiable that makes sure providers have the necessary patient data at their fingertips during telemedicine consultations.
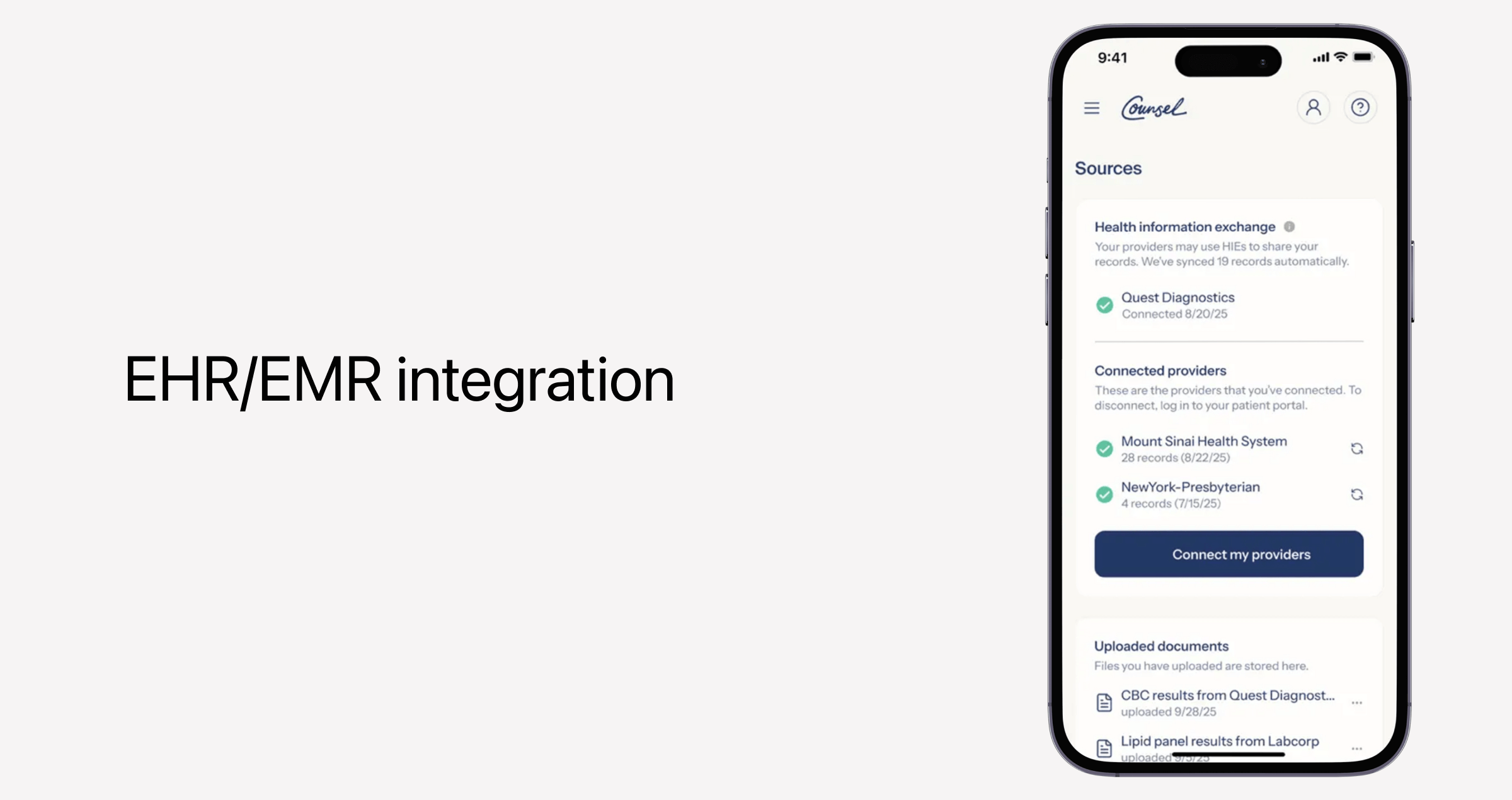
There’s a known level of complexity involved when it comes to this specific integration. First of all, telemedicine providers must consider synchronous appointments, which occur in real time, and asynchronous workflows that allow patients to log vitals and other data before or between virtual appointments. Also, EHR integration can be challenging to notch up because of differences in data formats, the lack of built-in interoperability in outdated medical records, and latency hurdles.
Appointment scheduling and management
Scheduling is a foundational feature for any telemedicine app. Patients expect telemedicine apps to provide a hassle-free, self-service way to book, reschedule, and cancel appointments. On the provider side, there’s a need for a unified system that keeps their calendars organized and synced across platforms and devices.
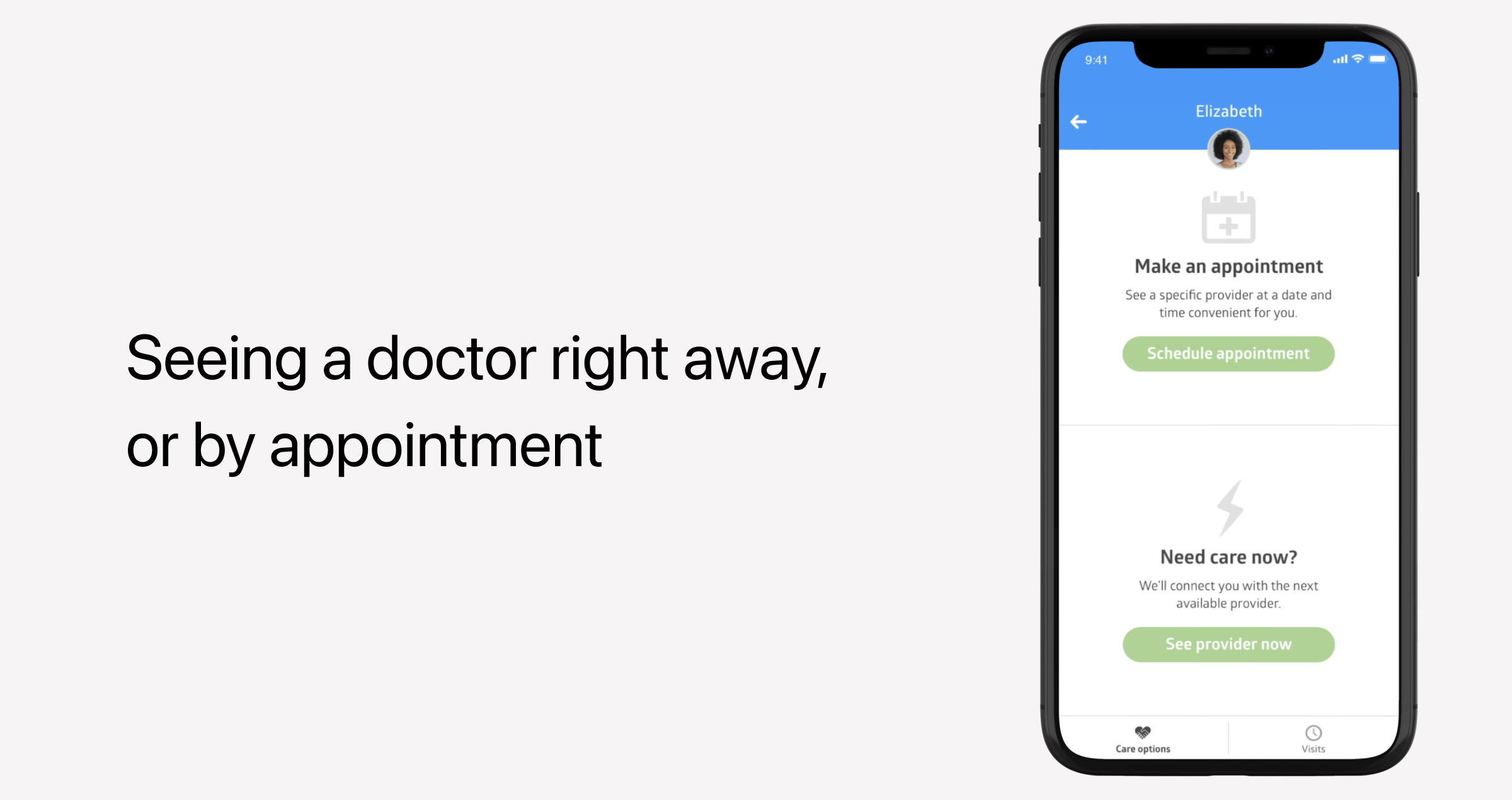
Some telemedicine software solutions also take it up a notch by enabling advanced scheduling features for patients, like waitlists and the ability to set up repeat appointments for ongoing treatment.
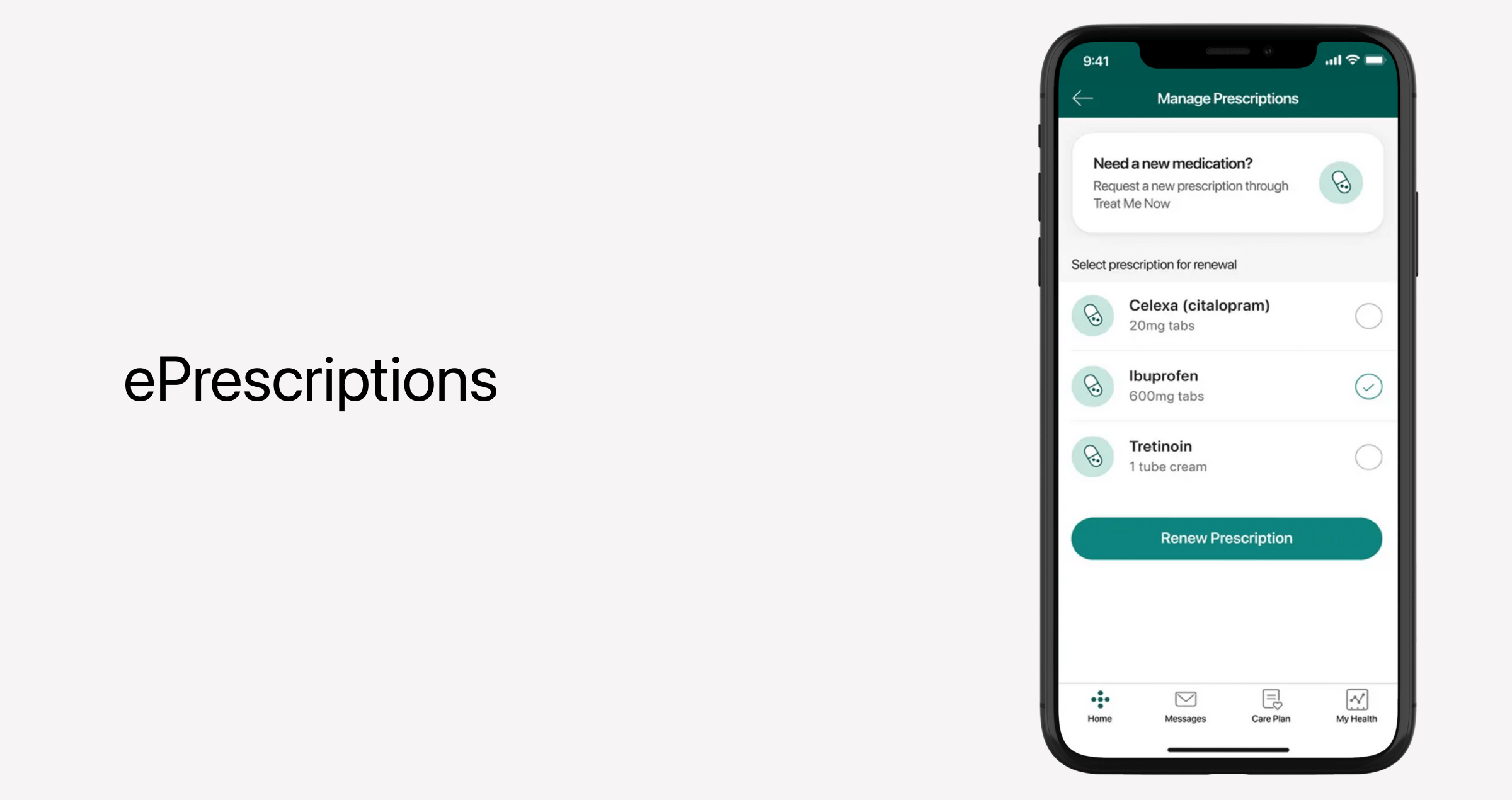
ePrescriptions
A telemedicine app usually allows patients to get their prescriptions online, without having to visit their primary care provider. At the same time, healthcare providers should be able to generate and send prescriptions directly to a patient’s pharmacy of choice. An MVP-level telemedicine app also often includes safety checks that flag potential issues like allergies or dosage limits.
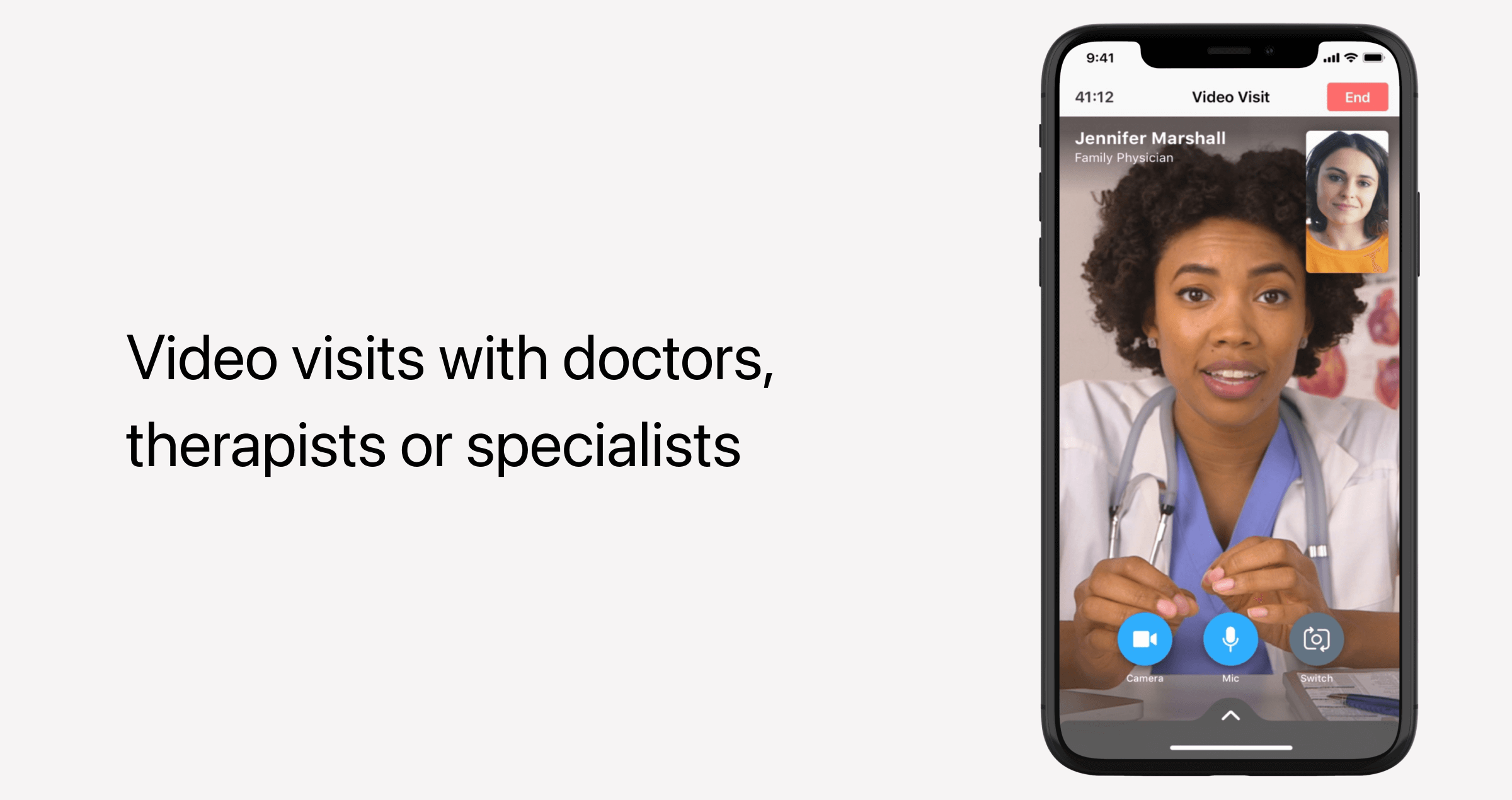
Video and audio consultations
HIPAA-compliant video and audio calls are cornerstone components of any telemedicine application. For an MVP, the focus should be on:
- The reliability of connection — Telemedicine apps usually rely on technologies like WebRTC to enable low-latency, high-quality communication even when the internet connection is slower than usual.
- The accessibility of virtual consultations — Make sure you also include an audio-only option in your telemedicine solution, as not all patients have reliable video bandwidth.
- HIPAA compliance — All video and audio streams must be encrypted end-to-end, while sessions must be stored on secure servers only. Among other things, the systems must maintain an audit log of sessions for compliance transparency.
Messaging system
Two-way HIPAA-compliant texting is another staple telehealth app functionality that keeps both sides of care connected between virtual visits. Besides, patients often have some follow-up questions — and asynchronous messages are a great option for that.
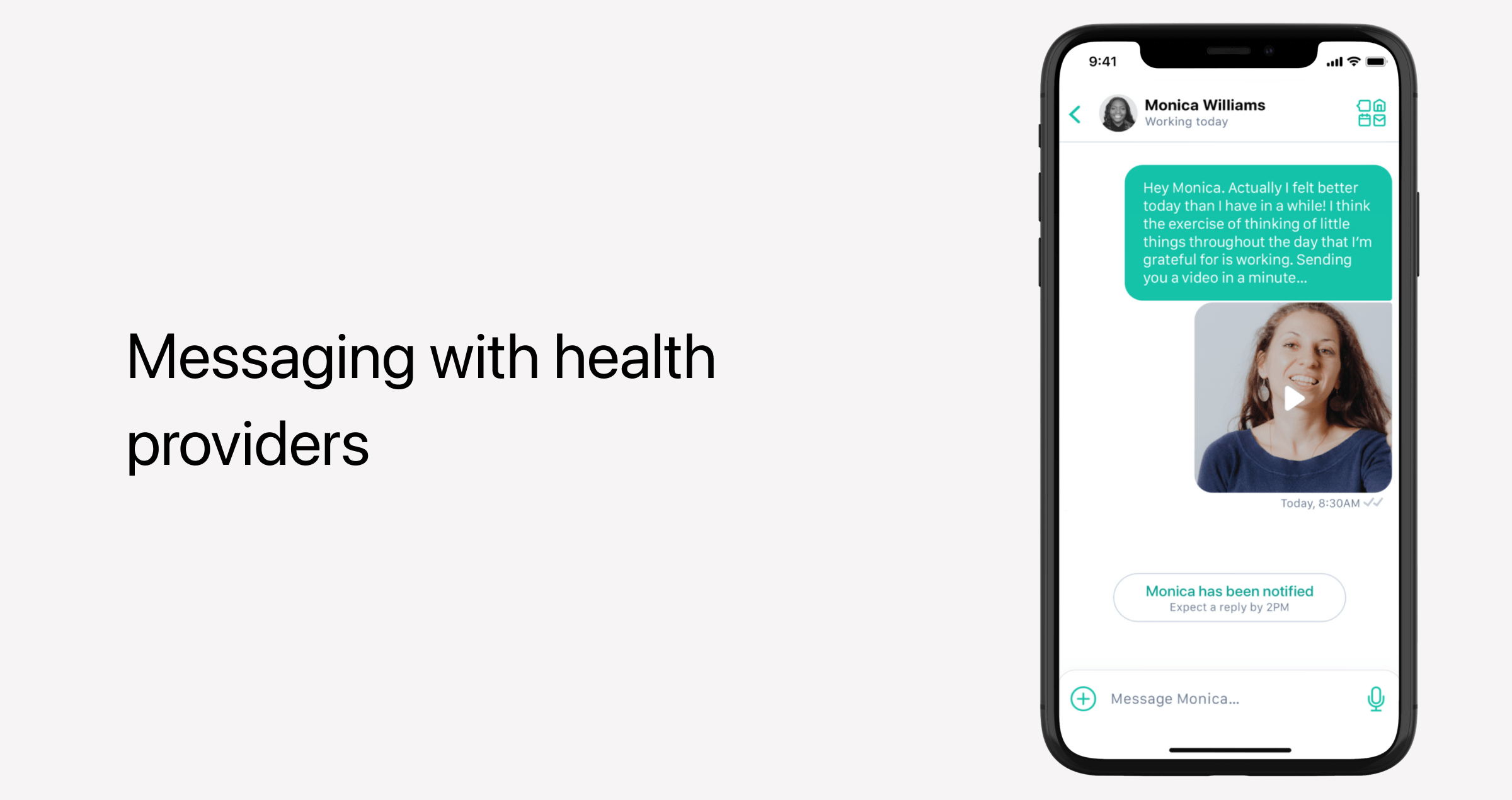
When it comes to MVP-level messaging, you need to make sure those are integrated:
- End-to-end encryption — The system must encrypt all messages between patients and healthcare professionals to protect personal health information.
- Attachment support — Patients and providers must be able to share documents, images, and lab results in the chat.
- Visit-specific chats — Messages are usually tied to a specific consultation or patient care episode to provide immediate context for providers.
Payment processing
Depending on the individual’s insurance plan and its coverage/benefits policy, some telemedicine visits can be covered, while others are not. Telemedicine providers should factor in both scenarios.
MVPs usually don’t have an integrated coverage verification since this feature is often postponed till a later product version. So, earlier telemedicine app versions ask patients to manually enter insurance information. But if your business model revolves around insurance coverage, integrating verification early becomes a must.
As for out-of-pocket payment options, telemedicine apps can offer HIPAA- and PCI DSS-compliant in-app payment options that allow users to pay medical bills via credit and debit cards. As an alternative, such apps can integrate with third-party integrated payment systems to handle card transactions.
Visit summaries and notes
After each consultation, both patients and providers should get a quick summary of what happened during the visit. In a minimum viable product, this feature is usually either non-automated or partially automated. Providers enter key information manually, with templates setting a structure for entering diagnoses, prescriptions, and other key information.
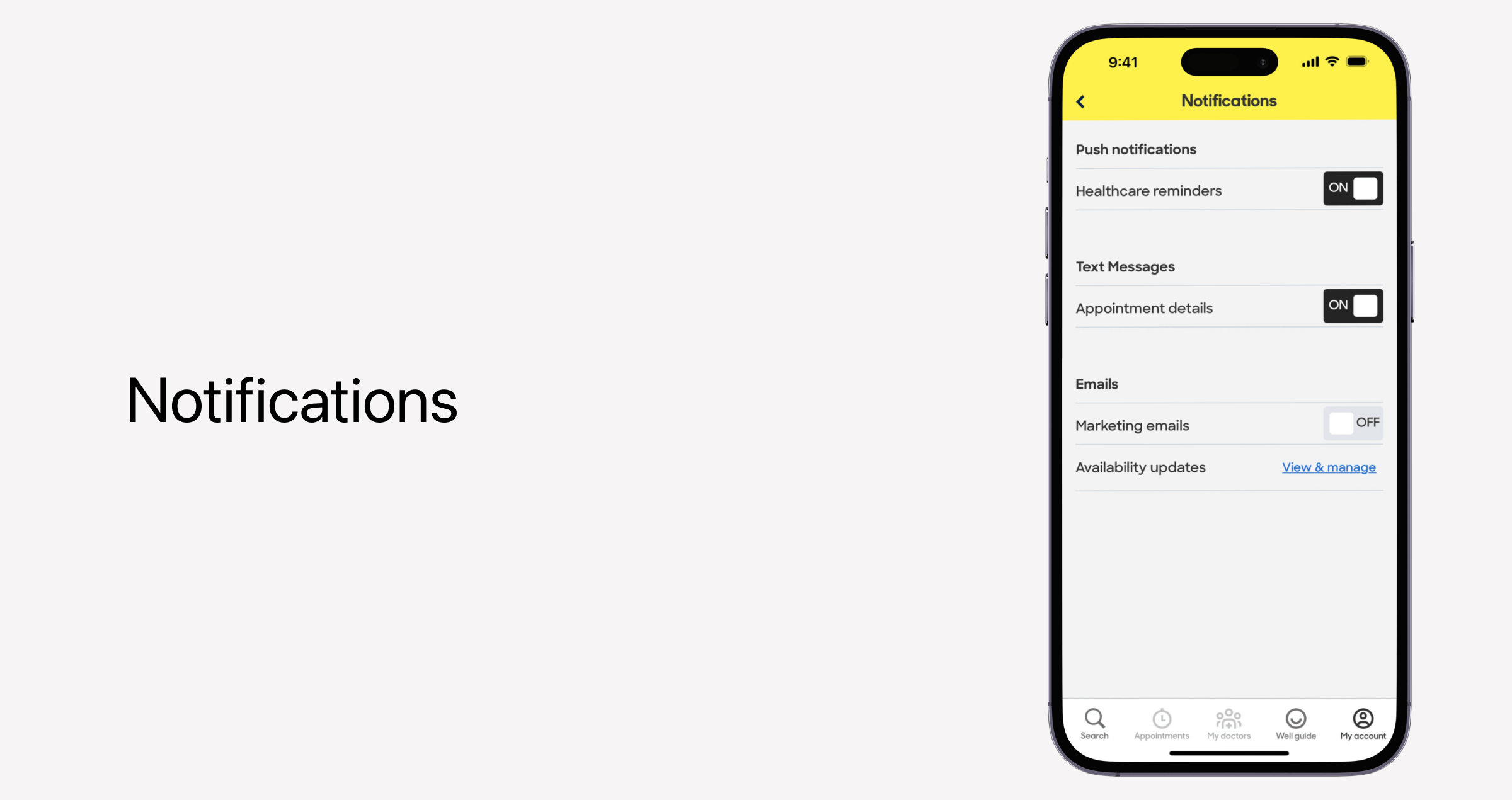
Notifications and reminders
Notifications remind users about upcoming consultations, new messages, test results, and relevant doctor recommendations. Notifications can come in the form of text messages, emails, or push notifications.
Advanced features for scaling your telemedicine apps to v1 and beyond
Back in the early days of the non-saturated telemedicine market, we used to classify AI-enabled workflows, IoMT integrations, and other cutting-edge features as sophisticated extras reserved for mature platforms that want to add advanced capabilities. It is still true to some extent, but the market has changed. Today, even startups tend to lead with advanced functionality to differentiate themselves in the market.
While we don’t recommend building everything from day one, we do advise laying the foundation for advanced features so that those can be easily integrated in later product versions.
Virtual waiting room
Virtual waiting rooms are unique, branded touchpoints that allow patients to check in virtually while they’re waiting to join their scheduled sessions. To invite the participant, telemedicine apps generate a secure and unique link that is sent prior to the session.
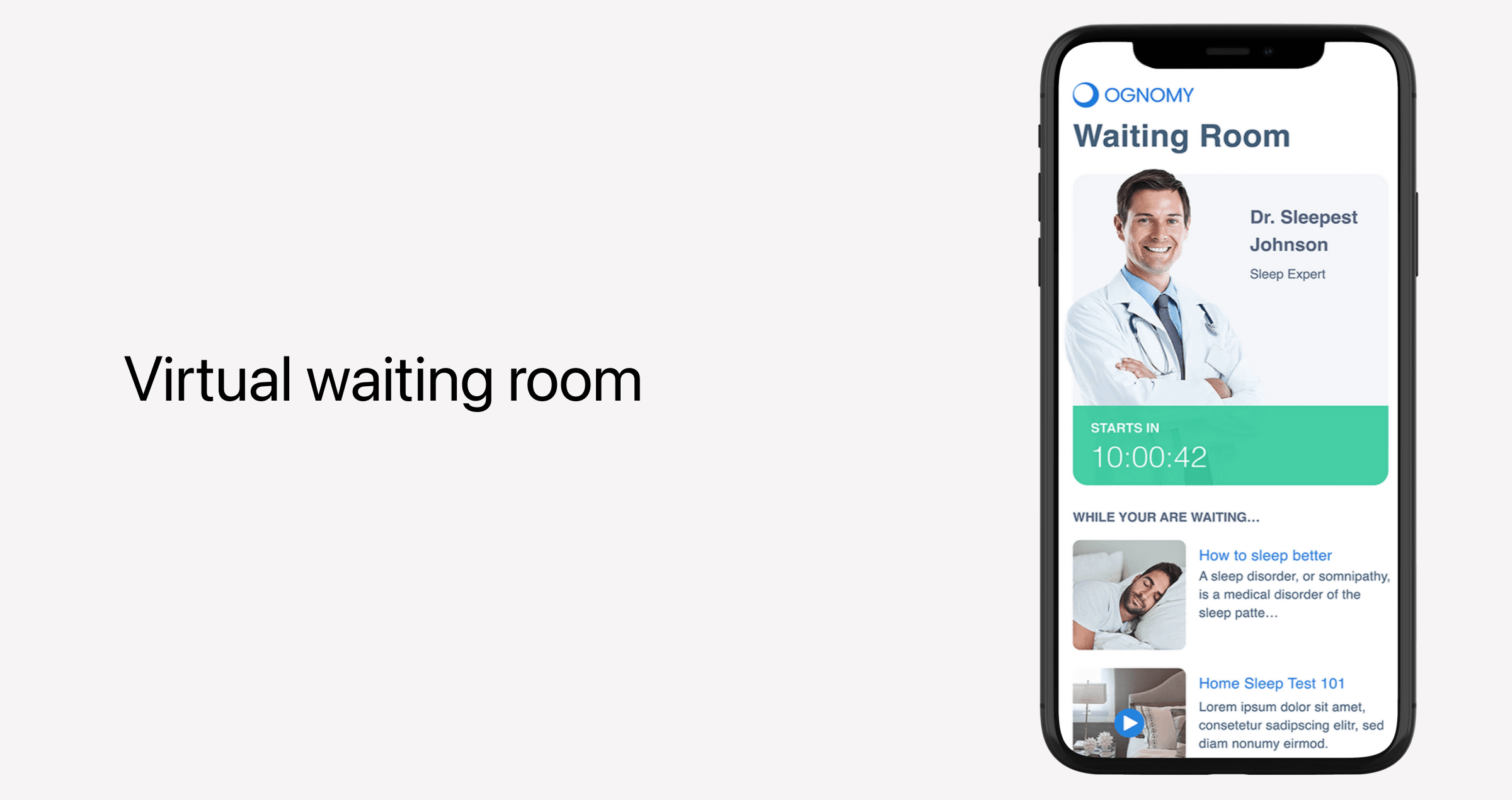
Virtual waiting rooms can serve different purposes, hence the varying features. Typical functionality includes:
- Paperwork management and pre-visit questionnaires — A dedicated virtual room allows patients to complete and submit the necessary information anytime ahead of their session.
- Engagement tools — Healthcare organizations can use this time to share tailored educational content, wellness tips, and other information that might be relevant to the patient’s condition.
- Queue management — Patients should see estimated wait times and their position in the queue.
AI-powered symptom checker or triage assistant
Powered by conversational AI and machine learning, this feature is integrated to collect and assess patient-reported symptoms and clinical decision points. Based on the result, the system presents a series of relevant recommendations or automatically routes patients to appropriate care. While human professionals aren’t always available 24/7, an AI assistant can show up for patients whenever they need assistance.
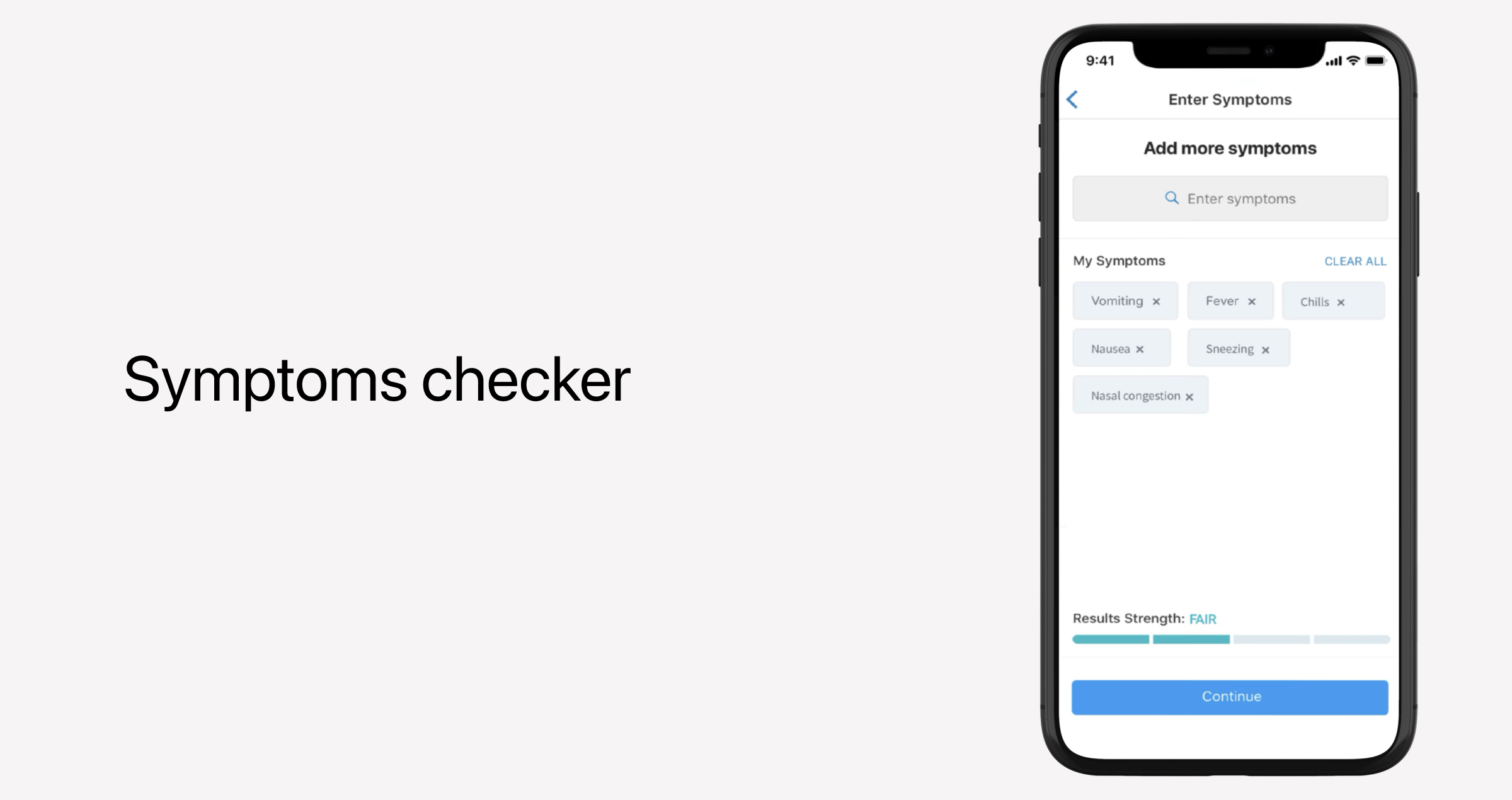
Along with instant guidance, AI triage assistants can also:
- Pre-populate patient records with structured symptom data, so providers won’t have to spend their time manually inputting this information.
- Prioritize cases based on severity and urgency, so that high-risk patients are seen sooner.
- Keep patients engaged in the care by answering follow-up questions, educating patients, and guiding them through pre-visit questionnaires.
Multi-party video calls
Multi-party video calls allow family members, caregivers, and multiple health care professionals to join the video consultation on a therapist-patient-family, interdisciplinary, or family-consultation format. Multi-party video calls foster patient support by ensuring everyone hears the provider’s recommendations directly.
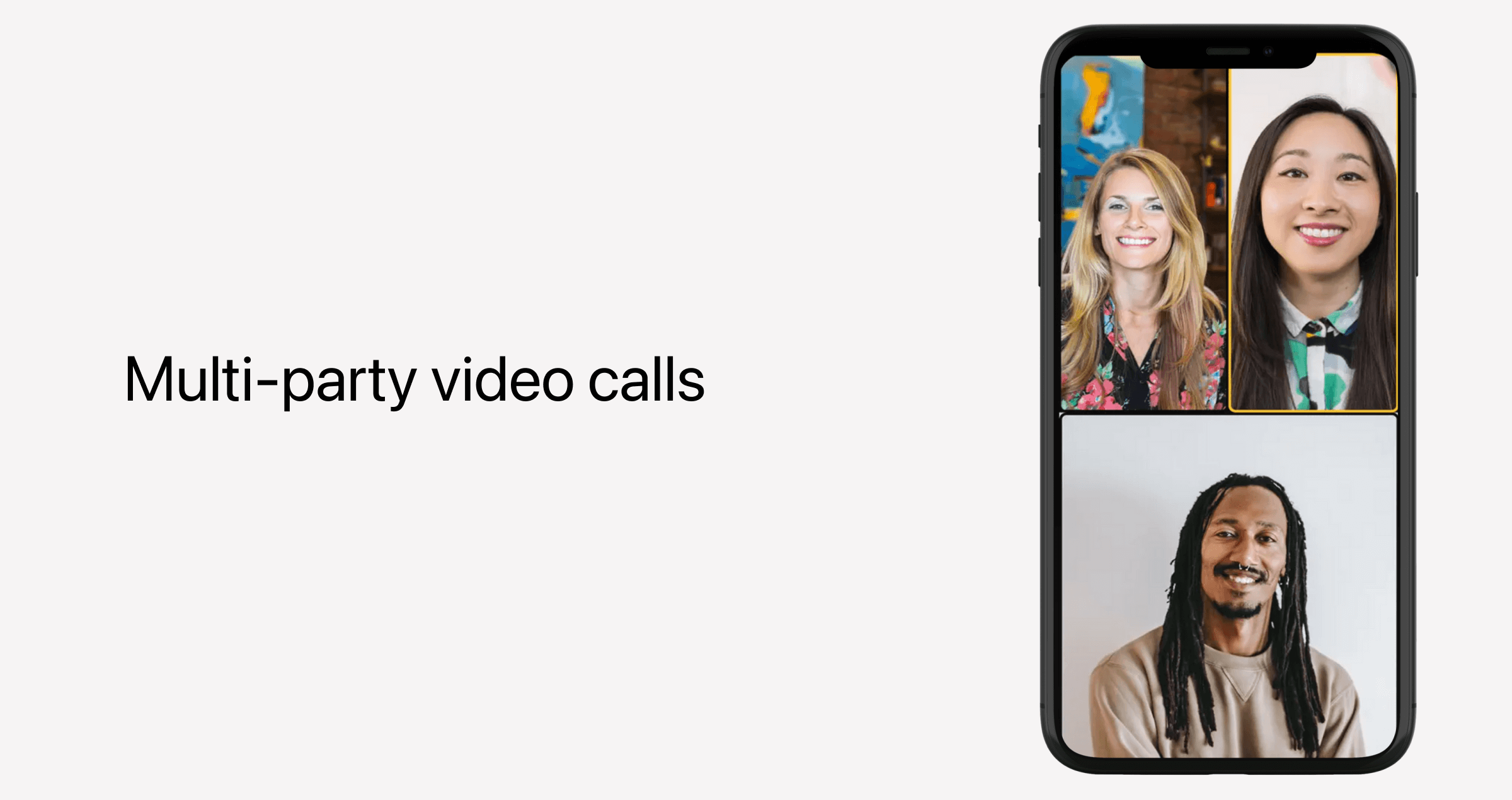
Of course, making it work smoothly for every party is a challenge. From a technical standpoint, multi-party video calls require role-based access and permissions, dynamic session management, and HIPAA-compliant encryption for every stream.
Multi-language support
Today, telehealth solutions cater to different patient populations, so virtual healthcare services should not only be high-quality but also culturally relevant. To that end, multilingual experience makes the communication clearer, care instructions easier to follow, and patients feel more heard and seen.
Multilingual experience goes beyond simple translation:
- UI and navigation localization — Menus, buttons, notifications, and other elements should feel intuitive for speakers of each language.
- Multi-language AI interactions — AI assistants, triage tools, symptom checkers, and other AI solutions should be developed taking into account the linguistic differences in medical terminology.
- Interpreter support for live sessions — Real-time subtitles or live translation during consultations will make sure there are no language gaps between patients and providers.
- Culturally sensitive content — All educational content should be adjusted based on the cultural norms and preferences.
Health data analytics
With healthcare data analytics tools, providers have algorithms automatically collecting, analyzing, and visualizing health and telemedicine data — to get a heads-up before any issues occur. The bigger your telemedicine platform grows, the more crucial this capability becomes.
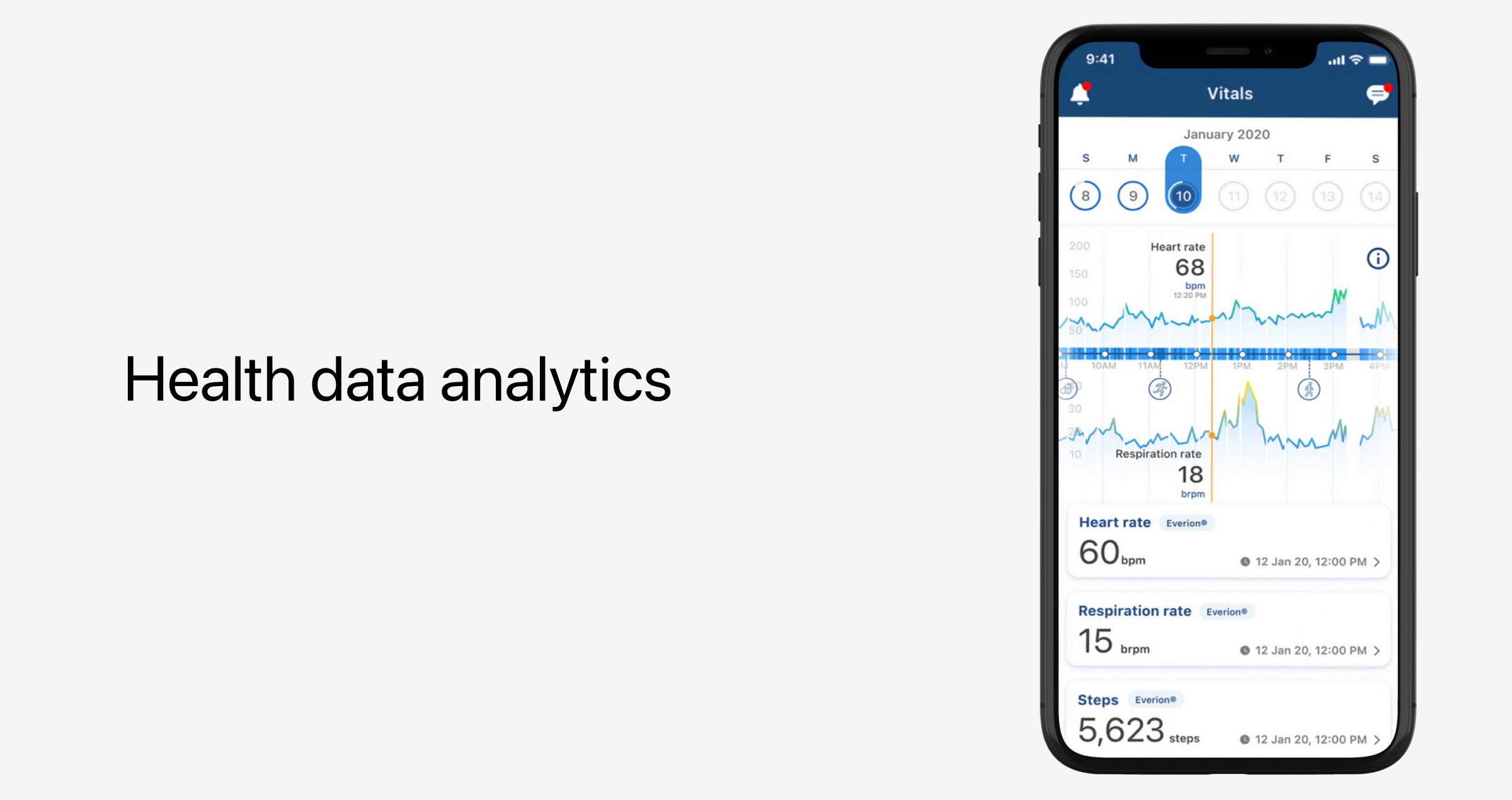
Dashboards allow clinicians and platform administrators to:
- Establish a real-time view of patient trends and health status — Dashboards highlight warning signs, summarize vital statistics, and show patients for follow-ups.
- Track population-level insights — The app will be able to tap into aggregated, anonymized data to identify trends like seasonal illnesses, medication adherence, and other patterns, without exposing individual health information.
- Inform evidence-based decisions — By leveraging analyzed data, providers can adjust treatment plans, medication management, and perform other tailored interventions, relying on objective information rather than assumptions.
Data analytics is considered an advanced feature for a reason. To implement it, developers need to integrate data from AI triage, patient-reported symptoms, EHRs, remote patient monitoring devices, and other healthcare apps to make sure the picture is complete.
IoMT and wearable device integration
Often, telemedicine applications grow to become a part of full-scale virtual care suites that rely on connected medical devices and wearables to gather longitudinal patient data. That makes Internet of Medical Things integration a logical next step.
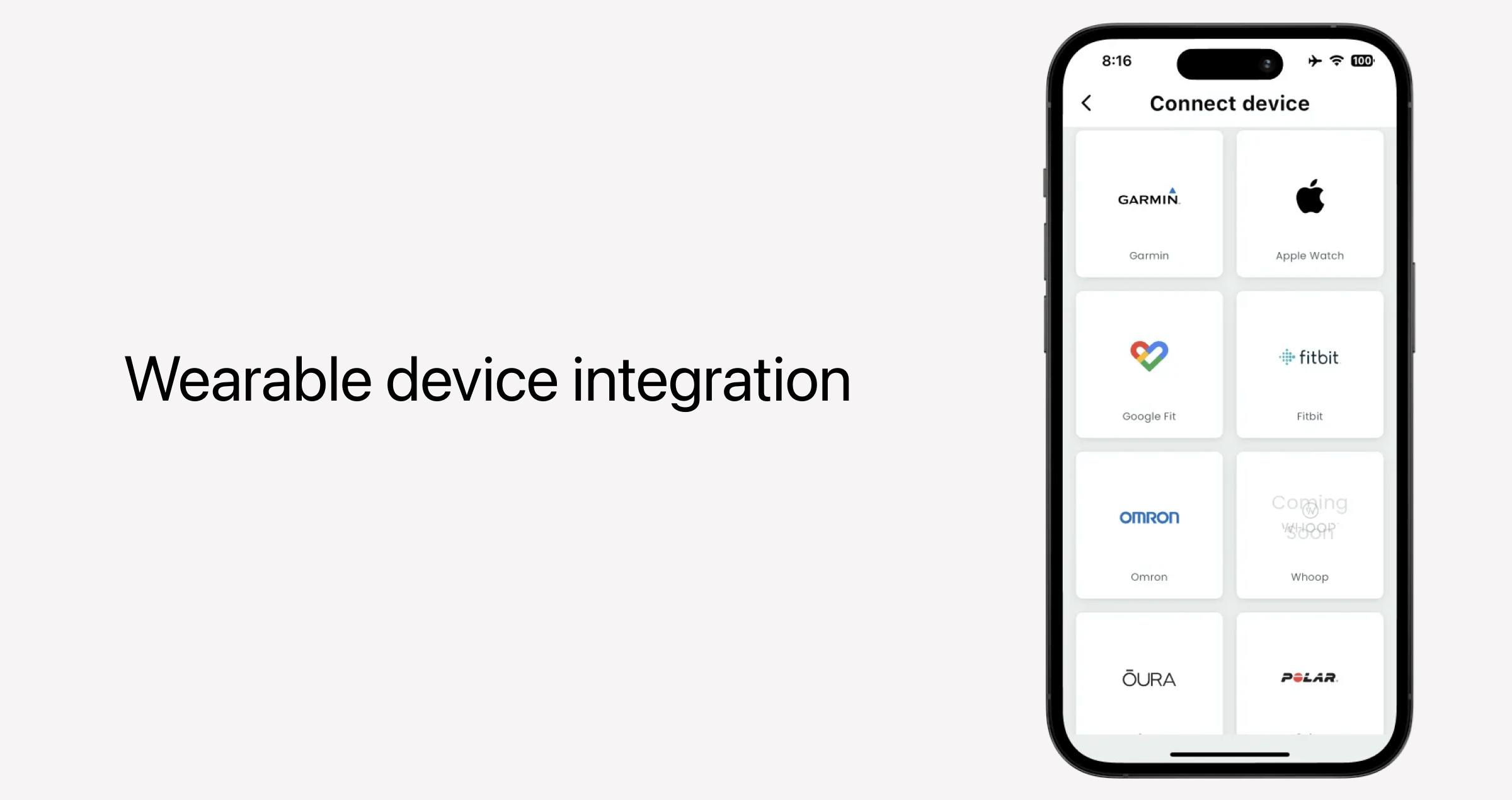
By collecting vital signs, activity levels, glucose readings, blood pressure, and other metrics in real time, telemedicine platforms can support continuous care programs for chronic disease management, mental health, and other conditions. Here, analytics go hand-in-hand, as the device data flows right into the dashboards.
Implementing this feature is technically challenging, as developers must address interoperability and data standardization challenges. Also, as the sensitive surface grows bigger, implementing this feature requires additional security measures to be baked into the platform.
Patient education
Another popular module, patient education, enables telemedicine providers to deliver a more empowering experience to patients. Educational content, preferably tailored to the patient’s condition, can include articles, videos, interactive modules, and other educational materials. These help patients get a better handle on their condition, treatment plans, and necessary lifestyle changes, which, ultimately, improve health outcomes for them.
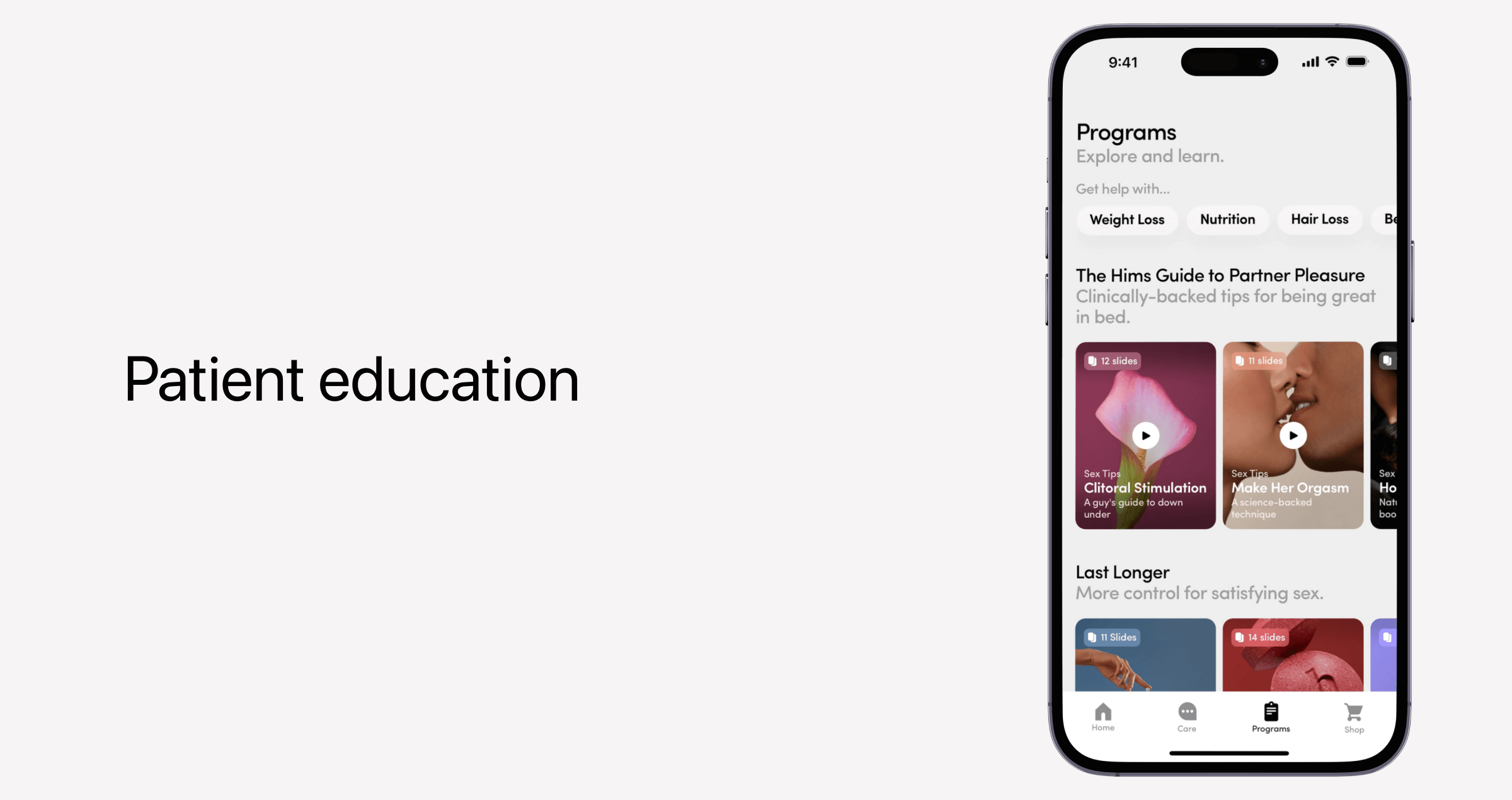
Also, educational content is a powerful engagement tool that keeps patients actively connected to the platform between sessions.
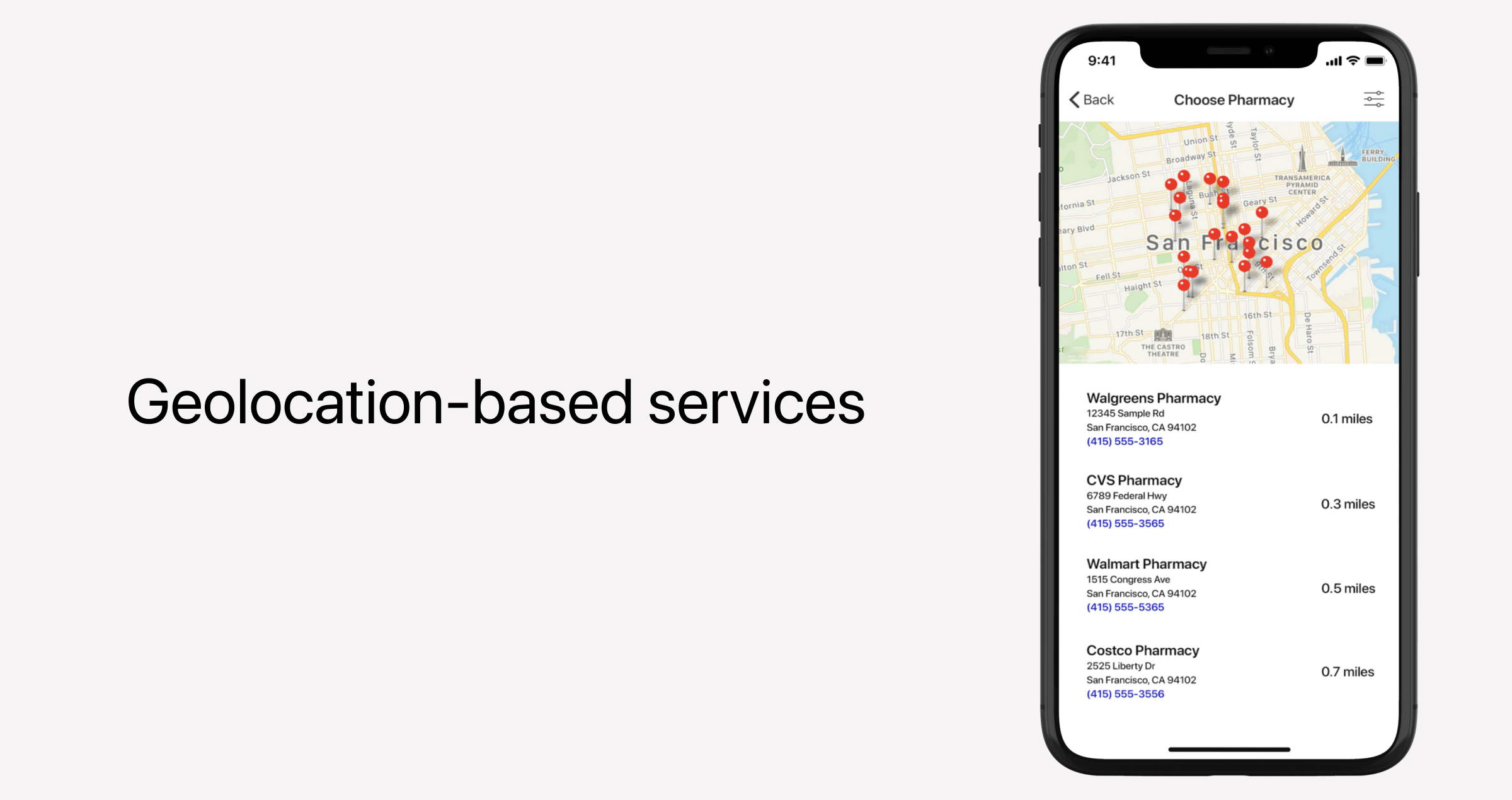
Geolocation-based services
The application can use the device's GPS or IP address to determine the patient's location and offer location-aware services, including:
- Matching patients with nearby providers.
- Sending location-based reminders, like picking up prescriptions or checking in for offline scheduled visits.
- Locating the nearest healthcare facilities, trauma centers, and ERs in case the patient needs emergency room visits.
Digital therapeutics support (DTx)
DTx tools are commonly known for rewiring healthcare delivery. Combined with telehealth technology, they extend beyond traditional telemedicine services to evidence-based therapeutic interventions, delivered directly on the patient’s device. We’re talking cognitive behavioral therapy, condition-specific programs, health progress tracking, adaptive care, and other personalized virtual medical services.
Technically, digital therapeutics are standalone software tools, often powered with AI and validated through clinical studies to earn their “evidence-based” credibility. They are always data-driven and often integrate with medical devices or wearables. DTx tools should also be interoperable with patient portals, clinician dashboards, and EHR systems, so that every bit of data becomes part of a bigger clinical story.
Integrated labs and diagnostics booking
Lab integration is a win-win add-on for both sides of care. For providers, this integration means they can send lab orders electronically and receive results directly within the EHR. For patients, it’s an ability to schedule lab tests, imaging, and other procedures and appointments right within a single interface. The lab data is then automatically mapped to the corresponding patient records and uploaded to the app and the patient portal.
Compliance and security considerations for telemedicine applications
The healthcare industry is a regulated field, and any app that takes on the responsibility of medical services and patient management is likely to be subject to multiple compliance requirements and health data standards. Telemedicine apps are not an exception.
Below, we’ve listed core compliance and security measures that most telemedicine applications include to lay a solid foundation for compliance with HIPAA, FDA, and other regulations. These should be baked into the platform early in the telemedicine app development process to avoid costly rebuilds later.
| Requirement | Why it matters | Implementation tips from Orangesoft |
|---|---|---|
| Data encryption | Prevents unauthorized users from accessing sensitive patient information | Use AES-256 for data at rest, TLS 1.2+ for data in transit |
| Secure authentication and access control | Makes sure only the right people see patient data | Implement multi-factor authentication, role-based access with least privilege, session management |
| Audit logs and monitoring | Catches unusual activity in its track and helps with compliance | Track logins, failed attempts, and data access events |
| Data storage and retention | Checks the regulatory boxes of storing and deleting patient data | Use compliant cloud storage, clear retention periods |
| Third-party integrations | Make sure connected apps do not introduce new security risks | Leverage only secure APIs and vetted SDKs, limit data sharing, perform regular security checks |
| Patient consent | Put and keep patients in control of their data | Provide clear privacy policies and opt-in forms |
Keep in mind that this is not an exhaustive list of measures, so it doesn’t automatically make your platform compliant. To get a full picture, we recommend consulting with experts.
Designing intuitive experiences, both for patients and providers
Telemedicine applications serve two very different audiences. On one hand, there’s a patient wary of the roadblocks and barriers that traditional healthcare systems throw at them. On the other hand, there’s a specialist doctor whose medical practice is filled with appointments, endless paperwork, and back-and-forth between screens.
Telemedicine applications should be thoughtfully designed around the needs and expectations of both sides.
For patients, this means:
- Accessible in-app experience — Live captioning, screen reader compatibility, high-contrast modes, and other accessibility features are a must for an inclusive patient experience.
- Intuitive navigation — Menus, search functions, flows, and other elements should be designed around validated user flows and tested early with real users.
- Transparency — Interfaces should feel safe, with explicit privacy policies, consent flows, and explanations of data usage reinforcing a sense of reliability.
For clinicians, the right design is more about ensuring the efficiency of care:
- Smooth workflows — The number of clicks that it takes doctors to complete tasks within the app should be kept to a minimum.
- Instant access to patient data — EHRs, lab results, visit notes, and other crucial data points should all be easy to find in one spot.
How we build and scale feature-rich, compliant telemedicine apps
Orangesoft is a software development company that specializes in healthcare software development. Over the years, we’ve developed telemedicine apps, remote patient monitoring platforms, engagement tools, and other software for medical organizations and innovative startups.
One of our clients, an established US-based healthcare provider, reached out to our team to scale its internal telehealth platform. The client was on a mission to bring their post-stroke patient monitoring program to other hospitals, but they lacked the internal capacity to expand the solution.
Our company focused on features that would deliver the most impact to users and align with our client’s business goals. Following an ISO-aligned development process, our tech specialists integrated telemedicine capabilities, patient management tools, care coordination capabilities, and other features into the platform. Every feature was implemented with strict adherence to HIPAA and FDA regulations.
Conclusion
It takes a fair amount of feature planning and prioritization to nail down the winning combination for a telemedicine app. Companies developing such solutions walk a fine line between delivering essential features that guarantee usability and compliance — and advanced extras that may, in fact, become essential differentiators in the market.
With the right approach and the right combination of features, telemedicine platforms can not only replicate the experience of in-person care but also improve it by making healthcare smarter, more accessible, and connected.
